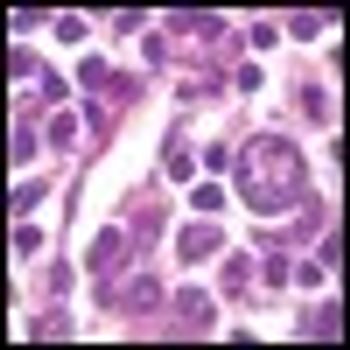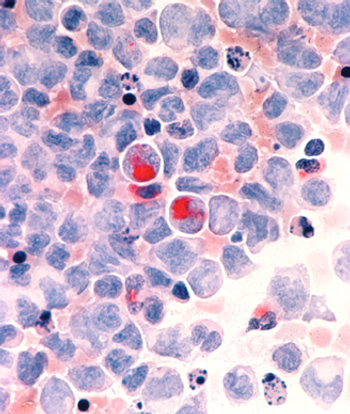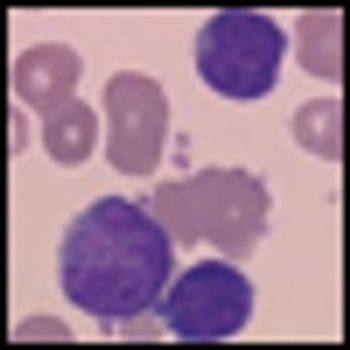
Three-year results from the ENESTnd trial show continued superiority of nilotinib over imatinib in patients with Philadelphia chromosome-positive chronic myeloid leukemia (CML) in chronic phase, according to a new paper published online ahead of print in Leukemia in June.