Neuroendocrine Tumors
Latest News
Latest Videos
More News

FDA Approves Lutathera for Gastroenteropancreatic Neuroendocrine Tumors
The US Food and Drug Administration approved lutetium Lu 177 dotatate (Lutathera) for the treatment of somatostatin receptor–positive gastroenteropancreatic neuroendocrine tumors in adults.

Patients with gastrointestinal neuroendocrine tumors with carcinoid syndrome are more than twice as likely to have certain pre-existing diagnoses compared with patients without carcinoid syndrome, according to the results of a study.

Proposed Liver Debulking Criteria for PNETs Could Improve Survival
Researchers are proposing the consideration of expanding criteria for liver debulking in pancreatic neuroendocrine tumors to include a threshold of greater than 70% debulking, intermediate grade tumors, positive margins, parenchyma-sparing resections, and extrahepatic metastases.
Pancreatic Neuroendocrine Tumors: State-of-the-Art Diagnosis and Management
In this review, we focus on the treatment of well-differentiated early and metastatic PNETs, emphasizing current controversies, recent advances in therapy, and the multidisciplinary approach required for optimal treatment.
BRAF Mutations May Be Driver of Colonic Neuroendocrine Carcinoma
A study exploring the genetic underpinnings of the newly classified high-grade neuroendocrine carcinoma has found that it is a rare but aggressive tumor with a high frequency of BRAF mutations.

QOL Analysis Supports Everolimus Use in Gastrointestinal, Lung NETs
Treatment of advanced, non-functional gastrointestinal or lung neuroendocrine tumors with everolimus resulted in improved progression-free survival with no relevant differences in health-related quality of life compared with placebo, according to an analysis of the RADIANT-4 trial.

The FDA has approved telotristat ethyl (Xermelo) tablets for the treatment of patients with carcinoid syndrome diarrhea that has not responded to somatostatin analogs alone.

Everolimus improved progression-free survival by 6 to 8 months compared with placebo in patients with advanced neuroendocrine tumors of the gastrointestinal tract.

Lutathera Slows Disease Progression in Midgut Neuroendocrine Tumors
A novel drug, 177Lutetium-DOTATATE (Lutathera), significantly lowered the risk for disease progression or death among patients with previously treated, advanced midgut neuroendocrine tumors.

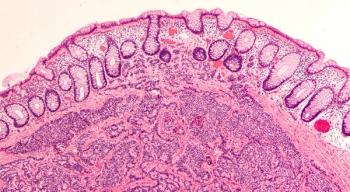
Small- and Large-Cell Neuroendocrine Cervical Cancer
Small- and large-cell neuroendocrine tumors of the cervix are exceedingly rare and exceedingly aggressive.

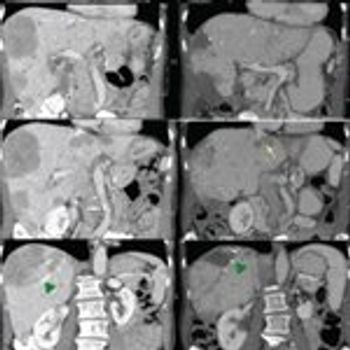
Primary Metastatic Small Intestinal Carcinoid Tumor Without Carcinoid Syndrome
Small intestinal “carcinoid” or well-differentiated grade 1 neuroendocrine tumors can have an insidious onset or be diagnosed serendipitously at the time of surgery, during the workup for another disorder, or during a screening test.

Nonfunctional neuroendocrine tumors of lung or gastrointestinal origin were safely and effectively treated with the mTOR inhibitor everolimus.

Patients with midgut neuroendocrine tumors had significantly delayed disease progression when treated with Lutathera compared with the current standard of care.

The US Food and Drug Administration approved lanreotide for the treatment of patients with gastroenteropancreatic neuroendocrine tumors.

Initial Treatment of Well-Differentiated Neuroendocrine Tumors
In patients with advanced, unresectable NETs, there are several treatment options; which of these may be considered depends on the site of origin of the tumor.

Small-Cell/Neuroendocrine Prostate Cancer: A Growing Threat?
Treatment-emergent small-cell/neuroendocrine prostate cancer is likely to become of increasing clinical relevance in the era of widespread use of potent androgen receptor–targeted therapies.
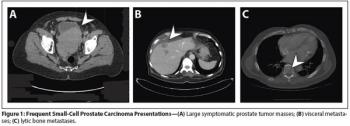
Neuroendocrine (Small-Cell) Carcinomas: Why They Teach Us Essential Lessons About Prostate Cancer
Aggressive variants of prostate cancer often take the form of neuroendocrine or small-cell carcinomas, which frequently lack androgen receptor expression and respond poorly to hormonal therapies.

Gastrointestinal Neuroendocrine Tumors: Slow but Steady Progress
In spite of recent encouraging developments in the setting of GI neuroendocrine tumors, many clinical questions remain to be answered and will be highlighted in this commentary.

The relative abundance of new data on the biological underpinnings of neuroendocrine tumors, combined with clinical trial data supporting new treatment options, is a clear sign of progress. Yet, as is so often the case, these recent studies have generated a multitude of new and different questions.
An Update on Gastroenteropancreatic Neuroendocrine Tumors
In this review, we summarize biologic, pathologic, and clinical aspects of gastroenteropancreatic-neuroendocrine tumors, focusing on recent advances in their treatment.

Researchers used an unbiased bioinformatics approach to identify a class of drugs currently used for non-cancer treatment that could be used to treat small-cell lung cancer, a cancer type for which there are few treatment options.

Dual Inhibition of VEGF and c-MET in Cancer Promises to Decrease Metastasis
A combined dual inhibition of vascular endothelial growth factor (VEGF) and c-MET is showing promise in preventing tumor invasion and metastasis. The data thus far are in a laboratory model of pancreatic neuroendocrine cancer.

Mutations in Genomic Integrity Gene Increase Hereditary Pancreatic Cancer Risk
Inherited mutations in the ataxia telangiectasia mutated (ATM) gene increase the odds of developing pancreatic cancer according to a new study. While there is predisposition for pancreatic cancer with up to 10% of cases occurring among families with a history of the disease, the genetic basis for this had not been previously discovered.

The review of surgical management of neuroendocrine tumors (NETs) of the gastrointestinal tract, authored by Huang, Poultsides, and Norton, is both comprehensive and accessible for readers of all backgrounds.

Surgical Management of Neuroendocrine Tumors of the Gastrointestinal Tract
This article reviews the surgical management of gastrointestinal neuroendocrine tumors, including the preoperative control of hormonal symptoms, extent of resection required, postoperative outcomes, and differing management strategies as determined by whether the tumor has arisen sporadically or as part of a familial disorder, such as multiple endocrine neoplasia type 1.