
Videos


Next steps in surgery for gastroesophageal cancer include offerings for patients with advanced disease, such as those with oligometastases.


Data from the GALAXY study in Japan may inform future use of total neoadjuvant therapy among patients with rectal cancer in the US.

The complicated nature of gastroesophageal cancer underscores the importance of collaboration between teams to safely treat patients with the disease.

Bodies like the NCCN must keep up with data related to ctDNA so that it can be incorporated in a measured manner, said Nicholas Hornstein, MD, PhD.

Described as a “doctor’s office on wheels,” the mobile unit is equipped with Wi-Fi and includes point-of-care PSA/imaging tests to help bring care to patients.
Explore the benefits of subcutaneous Amivantamab, including reduced infusion reactions and improved patient experience in cancer treatment.

Circulating tumor DNA may particularly help adjuvant treatment decision-making in stage II colon cancer, according to Nicholas Hornstein, MD, PhD.

The Million Strong Men Initiative is aimed at men at risk for prostate cancer who may be experiencing barriers to health care access.

Panelists discuss how results from antibody-drug conjugate trials, including those that fail primary endpoints, provide critical insights for refining sequencing strategies in hormone receptor–positive disease.

Explore the complexities of managing a Stage 3 gastric adenocarcinoma case, focusing on surgical options and perioperative treatment strategies.

This segment addresses one of the most rapidly evolving challenges in myeloma therapeutics: how to safely transition bispecific-treated patients between academic and community settings.
This case-based discussion illustrates the practical management of a 72-year-old patient with high-risk MDS and TP53 mutation.
Experts discuss the impact of daratumumab on smoldering myeloma, exploring survival rates, treatment options, and the importance of clinical trials.

Experts discuss the strengths and limitations of the Matterhorn study, highlighting advancements in immunotherapy for upper GI cancer and future research directions.

This segment focuses on the practical, multidisciplinary coordination required to safely administer bispecific antibodies.
Explore the AKELA trial's findings on patient characteristics and the impact of daratumumab on progression-free survival in myeloma treatment.

Panelists discuss how post-CDK4/6 endocrine strategies increasingly rely on molecular profiling to guide therapy selection and optimize benefit in resistant disease.
This segment explores the critical role of patient support programs, insurance navigation, and balancing the convenience of oral HMAs with ongoing clinical oversight.

Surgeons and radiation oncologists can collaborate to discuss expected toxicity and surgical outcomes among patients with resectable gastric cancer.

Explore the promising long-term outcomes of the IMERG trial, highlighting Emtresat's efficacy and safety for lower-risk MDS patients.

Explore real-world outcomes of hemoglobin treatment in low-risk MDS patients, comparing luspatercept and ESA therapies in a recent study.



Health care professionals emphasize the importance of patient education on adverse effects of amivantamab and lazertinib to improve treatment adherence and outcomes.
A study published in JAMA Network Open showed that patient trust in physicians and hospitals dropped from 71.5% in April 2020 to 40.1% in January 2024.
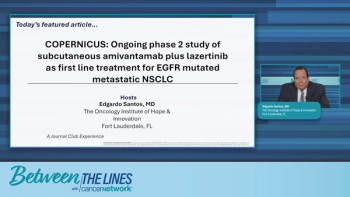
Explore the innovative Copernicus trial, evaluating subcutaneous Amivantamab plus Lazertinib for treating EGFR-mutated metastatic lung cancer.
Emphasizing critical thought over a conformity of thought in oncology may help prioritize and advocate for patients with cancer.
Explore the practical challenges of using oral hypomethylating agents, focusing on safety, access, and effective patient management strategies.

