Oncology NEWS International
- Oncology NEWS International Vol 10 No 8
- Volume 10
- Issue 8
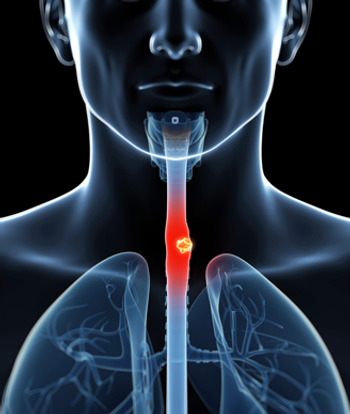
Reducing Toxicity of Combined-Modality Treatment for Esophageal Cancer
SAN ANTONIO, Texas-Although combined-modality therapy is considered the standard of care for patients with advanced esophageal cancer, the anatomical and physiological characteristics of the esophagus pose serious limitations on dose escalation. Cytoprotective strategies that might allow clinicians to circumvent these limitations were reviewed by Charles R. Thomas. Jr., MD.
SAN ANTONIO, TexasAlthough combined-modality therapy is considered the standard of care for patients with advanced esophageal cancer, the anatomical and physiological characteristics of the esophagus pose serious limitations on dose escalation. Cytoprotective strategies that might allow clinicians to circumvent these limitations were reviewed by Charles R. Thomas. Jr., MD.
The mucosal layer of the esophagus is a rapid turnover cell-renewal system and is dominant in early-responding tissue, Dr. Thomas noted. "Eventually there is some regeneration with these tissues if the dose isn’t too high. In mouse studies, large fractions produce vacuolization and thinning of the keratinized squamous cell layer by day 3, but there are foci of proliferating basal cells and regeneration of epithelium with concurrent areas of complete denudation by days 7 to 14, and near complete regeneration of esophageal layers by day 21," Dr. Thomas explained. He is associate professor and vice chairman of the Department of Radiation and adjunct associate professor of medical oncology at the University of Texas Health Science Center in San Antonio and the San Antonio Cancer Institute.
Acute changes in humans closely parallel the murine model. However, not all patients with acute esophagitis have direct pathologic correlation.
"Late changes are mostly related to muscle wall problems. The basal epithelial layer contains the target cells accounting for most acute radiation effects. Late effects are predominantly due to muscle cell layer compromise and to infiltration of fibroblasts and inflammatory cells into the esophageal muscle wall," Dr. Thomas said.
Higher Toxicity
Radiation Therapy Oncology Group study RTOG 85-01 randomized patients with esophageal cancer to radiation therapy alone vs chemoradiation therapy. Toxicity in a number of areas was much higher in patients who received the combined-modality regimen despite a benefit in survival.
"Intergroup protocol 0123 failed to show that dose escalation of radiation therapy in a multi-institutional setting could be done safely," Dr. Thomas said.
One strategy to reduce esophageal toxicity is to accurately determine biological target volume (BTV) by developing treatment-planning techniques that optimize functional and anatomical imaging data sets. Other strategies include 3-dimensional treatment planning and use of cytoprotective agents to protect normal tissues.
"One can get functional imaging tests such as PET scans. The idea is to delineate a BTV," Dr. Thomas said. "This may be the biological target that we need to aim at, and if that’s the case, our border would be a lot smaller than the traditional volume that we have been treating."
Studies with Amifostine
Dr. Thomas said that a pilot study of radiation plus subcutaneous amifostine (Ethyol) showed that amifostine significantly reduced mucosal toxicity. Patients treated with amifostine were also less likely to require radiotherapy delays.
The North Central Cancer Treatment Group is currently conducting a phase II trial (N0044) of preoperative radiation and chemotherapy (paclitaxel [Taxol], carboplatin [Paraplatin], and fluorouracil [5-FU]), with subcutaneous amifostine for locally advanced esophageal cancer. Patients are to receive amifostine at 500 flat dose SC, 20 minutes before radiation therapy.
Other cytoprotective strategies under investigation include glutamine, interleukin-15, melatonin, omega-3 fatty acids, transforming growth factor-beta, keratinizing growth factor, or gene therapy with intratumoral injection of manganese superoxide dismutase-plasmid/liposome (SOD2-PL).
Articles in this issue
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.