
Panelists discuss how the expanding volume of clinical data—both positive and negative—is increasing treatment complexity while reinforcing the need for individualized, patient-centered decision-making.

Your AI-Trained Oncology Knowledge Connection!


Panelists discuss how the expanding volume of clinical data—both positive and negative—is increasing treatment complexity while reinforcing the need for individualized, patient-centered decision-making.

Panelists discuss how toxicity monitoring and quality-of-life considerations must be adapted as potent therapies move into earlier-line and curative-intent settings.

Panelists discuss how identifying high-risk subgroups enables more precise selection of maintenance therapies that maximize progression-free survival while accounting for biomarker differences.

Panelists discuss how emerging neoadjuvant and adjuvant data in HER2-positive breast cancer are challenging traditional standards and supporting earlier use of highly effective agents.

Panelists discuss how results from antibody-drug conjugate trials, including those that fail primary endpoints, provide critical insights for refining sequencing strategies in hormone receptor–positive disease.

Panelists discuss how post-CDK4/6 endocrine strategies increasingly rely on molecular profiling to guide therapy selection and optimize benefit in resistant disease.

Panelists discuss how data from recent ESR1-mutant disease trials are influencing interpretation of survival end points, regulatory expectations, and real-world adoption of oral SERDs.

Panelists discuss how rapidly evolving guidelines are reshaping treatment pathways by preserving endocrine therapy as a backbone while introducing earlier use of combination regimens and ADCs.

Panelists discuss how sequencing targeted therapies after CDK4/6 inhibitors differs for patients with actionable mutations versus those without, incorporating evidence for rechallenge and combination strategies.

Panelists discuss how integrating both tissue and liquid genomic testing at diagnosis and progression improves detection of tumor heterogeneity and informs personalized treatment decisions in metastatic breast cancer.


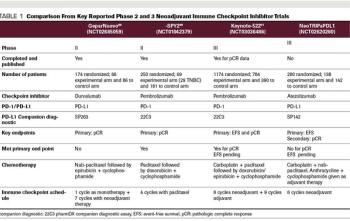
Experts review the current landscape and potential use of neoadjuvant chemotherapy with additional novel agents for patients with localized TNBC.

This video highlights an education session from SABCS on the management of locoregional recurrence in breast cancer.
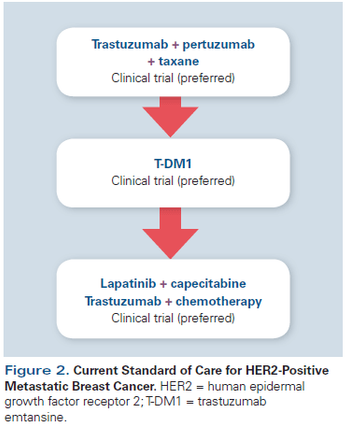
This review will summarize the current standard of care; key issues that arise when treating patients with HER2-positive disease; and developments in novel therapeutics, including small-molecule inhibitors, nanoparticles, immunotherapy, and agents targeting resistance pathways.

In this interview we discuss the effect of breast cancer treatments on fertility and the role oncologists can play in facilitating fertility care for their patients.

Here, we provide an in-depth review of the current evidence for the addition of ovarian suppression to adjuvant endocrine therapy, and we offer recommendations for clinical management.

In addition to the direct effects of primary tumors in bone, bone complications in cancer patients occur from metastasis to bone and through the effects of cancer-related treatments and conditions. Bone is a very common metastatic site for many cancers, including myeloma, melanoma, and breast, prostate, thyroid, lung, bladder, and kidney cancers. Metastatic bone lesions can be osteolytic (bone destruction resulting from increased bone resorption and reduced formation), osteoblastic (increased bone formation), or both.

Progress continues in the investigation of cytotoxicchemotherapy for breast cancer, and recentdata have yielded important new insights.

The use of adjuvant endocrinetherapy in early-stage breastcancer is thought to eradicatemicrometastatic disease that may leadto systemic recurrences. Until relativelyrecently, the standard adjuvantendocrine therapy option was tamoxifen.Data from the Early Breast CancerTrialists’ Collaborative Group(EBCTCG) overview analysis reporteda 50% reduction in the risk of relapseand a 28% reduction in the riskof death in estrogen receptor (ER)-positive patients treated with 5 yearsof tamoxifen.[1] This benefit was observedregardless of menopausal orlymph node status and whether or notpatients were receiving chemotherapy.There was no such benefit documentedin ER-negative cancersreceiving tamoxifen. Tamoxifen hasalso been associated with a 47% reductionin the risk of developing contralateralbreast cancer.[1]

With the advent of aromataseinhibitor use in the adjuvantsetting,[1] and the inceptionof trials examining their usefor breast cancer prevention, it seemsprudent to evaluate what we know todate about the long-term effects of these agents. Unfortunately, unlike selectiveestrogen-receptor modulators(SERMs)-in particular tamoxifen,[2]which has been used for over 15 yearsin patients with early-stage breast cancer-long-term data on the use of aromataseinhibitors are minimal.

Tamoxifen (Nolvadex), a selective estrogen-receptor modulator, or SERM, is currently the endocrine therapy of choice for all stages of hormone-responsive breast cancer. Only tamoxifen has been approved by the US Food and

The second edition of the Textbook of Uncommon Cancer is a useful resource for practicing oncologists who encounter unusual presentations of common tumors or esoteric subtypes of more common cancers. The text is laid out according to

New treatment strategies for advanced breast cancer have focused on both the development of new molecular targets in breast cancer cells, as well as improving the therapeutic index of presently available therapy. The

Symptoms related to estrogen deficiency are among the most common complaints that postmenopausal breast cancer patients bring to the attention of oncologists. Menopause develops in these patients either naturally or prematurely as a result of cancer chemotherapy and/or endocrine therapy.

Optimal management of locally advanced breast cancer (stage III) generally includes a combination of primary chemotherapy followed by surgery (if feasible), and local radiotherapy and adjuvant chemotherapy with or

Published: December 19th 2025 | Updated:

Published: March 1st 2007 | Updated:

Published: October 1st 1999 | Updated:

Published: September 1st 2001 | Updated:

Published: January 2nd 2001 | Updated:

Published: August 1st 1997 | Updated: