
Breast Cancer
Latest News

Latest Videos
CME Content
More News

An overview of unmet needs surrounding current treatment patterns for early-stage HR+ breast cancer.

Thoughts regarding how the addition of the Breast Cancer Index to the NCCN guidelines for HR+ breast cancer may likely impact extended adjuvant therapy and patient outcomes.
Dr Reshma L. Mahtani, of Sylvester Comprehensive Cancer Center, describes when and for whom she recommends genomic testing for HR+ breast cancer.
A review of recent updates to genomic testing guidelines by the National Comprehensive Cancer Network and important takeaways that impact treatment decisions for HR+ breast cancer in the extended adjuvant setting.

The rationale for treating early-stage HR+ breast cancer with extended adjuvant therapy and factors that impact treatment selection.

Insights into ongoing unmet needs in the individualized management of HR+ breast cancer and thoughts regarding future directions.

Identifying Patients for Extended Adjuvant Therapy With the Breast Cancer Index in HR+ Breast Cancer
Role of the Breast Cancer Index genomic index in therapeutic decision-making in the extended adjuvant setting in HR+ breast cancer.

A review of NCCN-recommended genomic assays and their impact on the management of HR+ breast cancer.

Best practices for the appropriate and timely use of genomic assays in clinical practice for patients with HR+ breast cancer.

Discussion of predictive and prognostic markers used to guide treatment decision-making in HR+ breast cancer.

The goals of adjuvant therapy versus extended adjuvant therapy for early-stage HR+ breast cancer and current treatment options available for each approach.

An optical coherence tomography–based imaging system was granted breakthrough device designation for detection of residual tissue during certain surgical procedures in patients with breast cancer.
CancerNetwork® spoke with Francesco Ravera, MD, PhD, during the American Association for Cancer Research Annual Meeting 2021 to discuss how results of a study aimed at determining pathological complete response in patients with locally advanced breast cancer by cell-free DNA may spare certain patients from needing further biopsies.

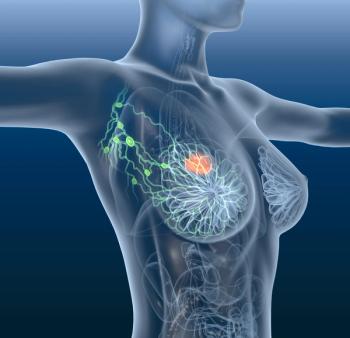
Recent guidelines have advised against routine use of sentinel lymph node biopsy and radiotherapy in patients over age 70 years with breast cancer, but a new study finds most patients still receive the interventions.
CancerNetwork® spoke with Francesco Ravera, MD, PhD, during the American Association for Cancer Research Annual Meeting 2021 to discuss results of a study aimed at determining pathological complete response in patients with locally advanced breast cancer by either cell-free DNA assessment or traditional MRI.

CancerNetwork® spoke with Francesco Ravera, MD, PhD, during the American Association for Cancer Research Annual Meeting 2021 to discuss a study that looked at cell-free DNA assessment compared with traditional MRI for determining pathological complete response in patients with locally advanced breast cancer.

“It’s a time for great hope with breast cancer, given the number of agents being evaluated now.” –Sara A. Hurvitz, MD
The clinical benefit rate of the neratinib plus fulvestrant combination treatment did not meet the predefined efficacy threshold, but was active in heavily pretreated patients with estrogen receptor-positive, metastatic breast cancer.

During a presentation at the American Association of Cancer Research Annual Meeting 2021, Ben L. Kong, PharmD, described the SMMART program, which pairs genetic and clinical information to find the best therapies for patients with breast cancer who progress on standard therapies.

TAS-117 showed limited clinical efficacy in treating patients with ovarian cancer harboring PIK3CA E545K mutations and in those with breast cancer harboring PIK3CA H1047R and Akt1E17K mutations.
An analysis of real-world outcomes in a cohort of patients treated in mostly community settings showed that palbociclib plus letrozole improved both progression-free and overall survival in women with hormone receptor–positive, HER2-negative metastatic breast cancer.

Following last year’s accelerated approval designation, the FDA granted regular approval to sacituzumab govitecan to treat patients with triple-negative breast cancer.
The next-generation cryoablation technology ProSense was granted breakthrough device designation to treat certain patients with T1 breast tumors.

A study from JAMA Oncology investigated the association between BRCA1/2 pathogenic variants and risk-reducing salpingo-oophorectomy for breast cancer, concluding that a benefit exists for women in the immediate 5 years post-surgery.

Data presented at the Society of Surgical Oncology 2021 International Conference on Surgical Cancer Care found that breast pCR was predictive of nodal pCR for patients with HER2-positive and triple-negative breast cancer treated with chemotherapy.











































