Plinabulin in combination with pegfilgrastim reduced the incidence of chemotherapy-induced neutropenia, compared with pegfilgrastim alone, in patients with breast cancer undergoing chemotherapy with docetaxel, doxorubicin, and cyclophosphamide.

Your AI-Trained Oncology Knowledge Connection!

Plinabulin in combination with pegfilgrastim reduced the incidence of chemotherapy-induced neutropenia, compared with pegfilgrastim alone, in patients with breast cancer undergoing chemotherapy with docetaxel, doxorubicin, and cyclophosphamide.
The breast medical oncologist and researcher discussed how the addition of chemotherapy to endocrine therapy showed clinical benefit in premenopausal, lymph node-positive, HR-positive, HER2-negative breast cancer.
Research presented at the 2020 SABCS found providers planned to use neoadjuvant endocrine therapy for as little as possible until surgery was available for patients with estrogen receptor positive breast cancer.
The GP2/GM-CSF combination demonstrated a 100% disease-free survival at 5 years for patients with HER2/neu 3–positive disease who received adjuvant trastuzumab.
For women with heavily pretreated, postmenopausal advanced or metastatic estrogen receptor (ER)–positive breast cancer, amcenestrant prompted antitumor activity.

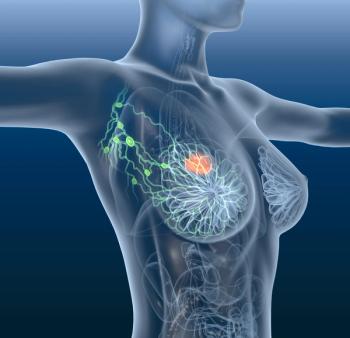
The study found that favorable outcomes after treatment with lapatinib (Tykerb) were demonstrated by early declines in circulating tumor cell counts (CTCs) in patients with metastatic breast cancer who initially had HER2-negative primary tumors but positive HER2 CTCs.
Fewer deaths and improved cumulative incidence of central nervous system recurrences were shown at 8 years of follow-up with adjuvant neratinib (Nerlynx) compared with placebo in patients with early-stage HER2-positive breast cancer following trastuzumab (Herceptin)-based therapy.

Combination treatment with alpelisib (Piqray) and letrozole (Femara) sustained efficacy and did not result in any new safety signals in patients with PIK3CA-mutant HR-positive, HER2-negative advanced breast cancer who received prior treatment with the combination of a CDK4/6 inhibitor and fulvestrant (Faslodex).

Women who survive breast cancer may have more difficulty in becoming pregnant when compared to the general population, and have a risk of preterm labor, but most deliver healthy babies and experience no detrimental effects on their long-term survival.

The combination of oral paclitaxel and encequidar has the potential to be an effective treatment for patients with radiation-associated breast angiosarcoma.
Adhering to a diabetes risk reduction diet improved survival for women with stage 1 to 3 breast cancer compared to women who did not follow this specific diet.
Data from the APHINITY trial suggested that patients with early breast cancer with a HER2 single-activated pathway determined by molecular subtyping using BluePrint assay demonstrated a trend for greater benefit with adjuvant pertuzumab (Perjeta) therapy.

Treatment with the combination of oral paclitaxel and encequidar was found to be associated with greater efficacy in patients with metastatic breast cancer, as well as lower rates of chemotherapy-induced peripheral neuropathy, compared to intravenous paclitaxel.

Behavioral interventions were found to help young breast cancer survivors in reducing their depressive symptoms.
Ribociclib plus endocrine therapy continued to show a significant overall survival improvement, while delaying subsequent chemotherapy for patients with HR+/HER2-negative breast cancer.
An analysis of tamoxifen versus anastrozole showed no significant difference in terms of disease recurrence in postmenopausal women with locally excised ductal carcinoma in situ; however, the findings may highlight the understanding of associated toxicities.

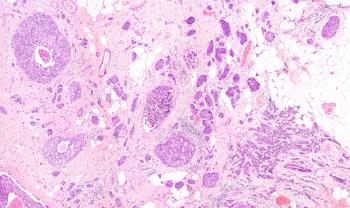
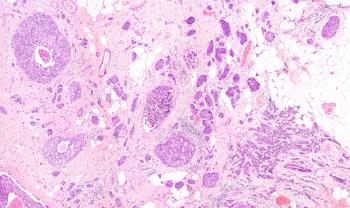
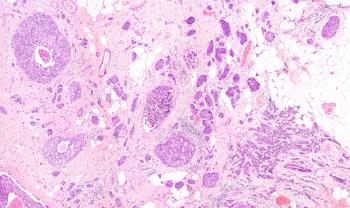
PreciseDx, an artificial intelligence–digital breast cancer risk discrimination platform, was able to classify patients with Oncotype Dx low-risk recurrence scores with high accuracy using only hematoxylin and eosin stain images and limited clinical data.

After breast-conserving surgery and adjuvant endocrine therapy, whole breast irradiation can be omitted from the treatment journey of low-risk, older patients with pT1-2 tumors (≥3 cm) who are on local control at 10 years.
A retrospective exploratory analysis found that intrinsic tumor subtype was associated with prognosis in patients with hormone receptor–positive, HER2-negative advanced breast cancer who received the CDK4/6 inhibitor ribociclib.

Treatment with oral paclitaxel, compared with the intravenous formulation, in combination with encequidar led to an estimated 26.5% reduction in the risk of death in patients with metastatic breast cancer, according to updated phase 3 findings of the KX-ORAX-001 trial.
A poster presented at the 2020 San Antonio Breast Cancer Symposium found a trend towards less frequent care refusal when a safety net hospital introduced nurse breast navigators.

Study results suggested that while chemotherapy-induced nausea/vomiting (CINV) can be treated, there is potential for it to return, especially for patients for whom CINV treatment did not work the first time around.
Research presented at the 2020 San Antonio Breast Cancer Symposium highlighted the need for reliable information to address the educational and psychosocial needs of patients with newly diagnosed metastatic breast cancer.
Chemotherapy plus endocrine therapy improved 5-year invasive disease-free and overall survival in premenopausal women with HR–positive, HER2-negative, lymph node–positive breast cancer and a recurrence score between 0 and 25.
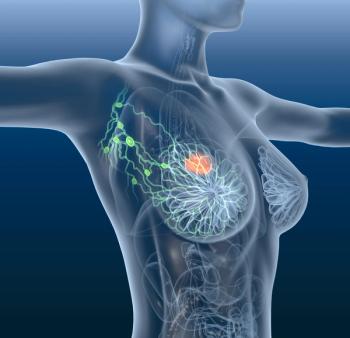
The use of serial circulating tumor cell enumeration was confirmed to strongly predict overall survival outcomes in patients with metastatic breast cancer.