Myeloproliferative Neoplasms
Latest News
Latest Videos
CME Content
More News

In this interview we discuss clinical developments in essential thrombocythemia, polycythemia vera, and myelofibrosis, as well as the latest treatment options.
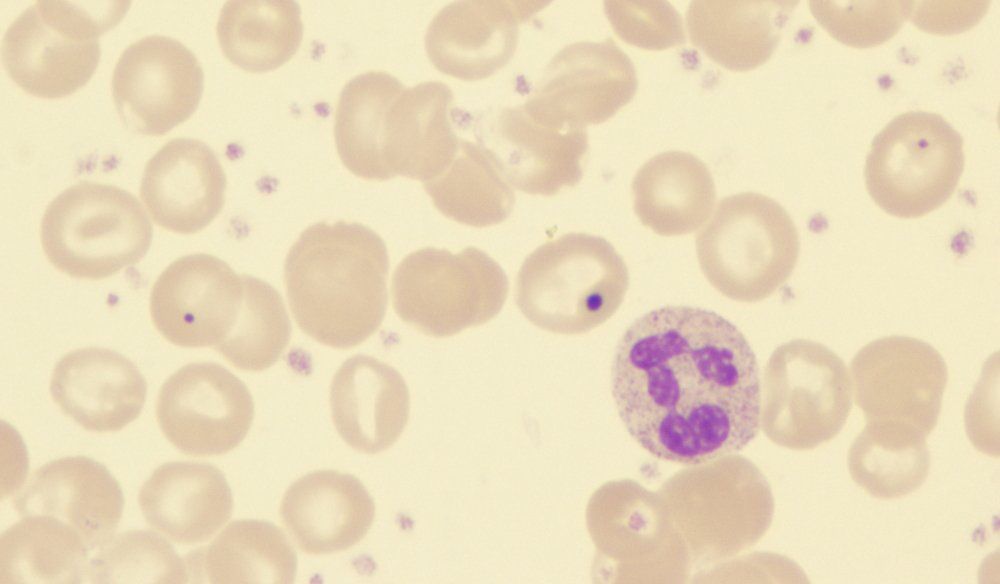
A 60-year-old man with a history of coronary artery disease and JAK2 V617F–positive polycythemia vera presented to our bone marrow transplantation clinic with progressive fatigue, splenomegaly, and cytopenias.

In this interview we discuss symptoms and prognosis for patients with polycythemia vera and essential thrombocythemia and the treatment of myelofibrosis.

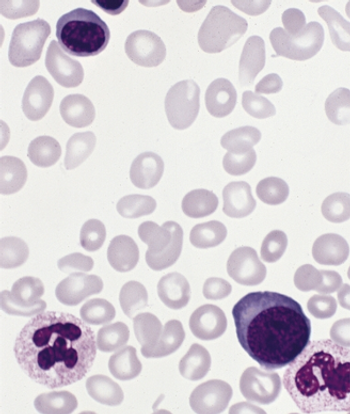
Myeloproliferative neoplasms are a group of clonal myeloid cell–derived disorders characterized by myeloproliferation without dysplasia, bone marrow hypercellularity, and predisposition to thrombosis, hemorrhage, and bone marrow fibrosis.

A new study has confirmed that the symptom burden of patients with polycythemia vera is substantial, and is independent of a patient’s disease features.

A study found that patients with myeloproliferative neoplasms have a higher overall mortality rate due to death from hematologic malignancies and infections.
New data indicates that the order in which people acquired certain somatic mutations influenced several clinical features of myeloproliferative neoplasms.
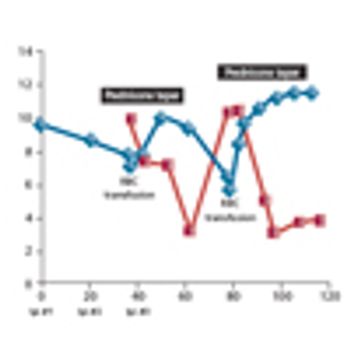
Ruxolitinib was significantly better than the best available therapy in a phase III, open-label trial of patients with polycythemia vera who were resistant to or intolerant of hydroxyurea.

A rare subtype of disease known as atypical chronic myeloid leukemia (aCML) has been shown to be clinically distinct from a related condition known as unclassifiable myelodysplastic/myeloproliferative neoplasm.

In a late-breaking abstract presentation, Thorsten Klampfl, PhD, of the CeMM Research Center for Molecular Medicine of the Austrian Academy of Sciences in Vienna, presented data from a whole exome study of primary myelofibrosis patients, identifying a new specific molecular mutation

Palliation is a laudable concept and an important goal in the therapy of all patients with malignant disease. Unfortunately, in the current day and age, the adjective “palliative” is being used in a derogatory manner that suggests palliation of suffering somehow lessens the importance or impact that such a therapy has upon individuals with the disease.

By inhibiting inflammatory cytokines and controlling the signs and symptoms of myelofibrosis, the patient’s body condition improves as the disease is kept under good control. Ultimately, prolonged exposure of a patient with myelofibrosis to ruxolitinib at a clinically effective dose results in prolongation of the his or her life.

In this article, we provide updated data on ruxolitinib therapy for patients with myelofibrosis and offer expert opinion on the appropriate use of this agent in the community practice.
Is it time to revisit the therapeutic role of interferon alfa2 (IFN-α-2) in early myelofibrosis (MF) since new data show promising results? Silver et al from Weil-Cornell Medical College in New York has recently published the results of a prospective study, which used IFN-α-2 in the treatment of 17 patients with low and intermediate-1 risk categories, and >80% of patients showed either response or had stable disease with 2 patients achieving complete remission (CR), and seven partial remission (PR).

Patients with myelofibrosis experienced relief from pain, fatigue, and other symptoms associated with enlarged spleens after treatment with a JAK1 and JAK2 inhibitor, according to study results from Houston’s M.D. Anderson Cancer Center.

Research presented at the 51st Annual Meeting of the American Society of Hematology (ASH) in New Orleans introduced potential new treatment options and improved diagnostic methods for patients suffering from acute promyelocytic leukemia (APL), chronic myeloid leukemia (CML), infant acute lymphoblastic leukemia (ALL), and myelofibrosis that are based on a better understanding of the underlying genetic causes of these conditions.

NEW ORLEANS-A new treatment for patients who are severely debilitated by myelofibrosis offers hope of a return to normal daily life. Preliminary studies with an oral drug INCB018424 that targets the Janus-activated kinase (JAK) 2 gene appears to markedly reduce the swelling of the spleen and sometimes the liver, which can, in turn, can change patients’ quality of life.

HOUSTON-The farnesyl transferase inhibitor R115777 (tipifarnib, also known as Zarnestra) produced an overall response rate of 33% in patients with chronic myelogenous leukemia (CML) and decreased splenomegaly in most patients with myelofibrosis, but was not effective in multiple myeloma, reported Deborah Thomas, MD, at the 43rd Annual Meeting of the American Society of Hematology. Dr. Thomas is assistant professor in the Department of Leukemia at The University of Texas M. D. Anderson Cancer Center in Houston.

Myeloproliferative disorders originate in the clonal expansion of a transformed pluripotential hematopoietic progenitor cell. This results in a group of syndromes that include polycythemia vera, essential thrombocythemia,

Myeloproliferative disorders originate in the clonal expansion of a transformed pluripotential hematopoietic progenitor cell. This results in a group of syndromes that include polycythemia vera, essential thrombocythemia,

Myeloproliferative disorders originate in the clonal expansion of a transformed pluripotential hematopoietic progenitor cell. This results in a group of syndromes that include polycythemia vera, essential thrombocythemia,

NEW YORK-Bone marrow ron-geur can free some patients with advanced myelofibrosis of the need for blood transfusions, Richard T. Silver, MD, clinical professor of medicine, Weill Medical College of Cornell University, said at the Chemotherapy Foundation Symposium XVIII. Dr. Silver’s major collaborators in the study were Dr. Malcolm Moore, a noted cell biologist at Memorial Sloan-Kettering Cancer Center, and Dr. Edward Athanasian, an orthopedic surgeon at the Hospital for Special Surgery, New York.