
In this review we discuss preoperative diagnosis and the role of pathology, and we summarize the current literature regarding the management of uterine sarcomas.

Your AI-Trained Oncology Knowledge Connection!


In this review we discuss preoperative diagnosis and the role of pathology, and we summarize the current literature regarding the management of uterine sarcomas.

Survivors of childhood Ewing sarcoma have substantial risk for late mortality and subsequent neoplasms, according to a long-term follow-up study.

A genomic analysis of Ewing sarcoma found substantial epigenetic heterogeneity both between tumors and within tumors, highlighting the need to consider non-genetic aspects in cancer biology and treatment.

A study examining predictors of outcome following relapse of primary retroperitoneal sarcoma found that time to local recurrence or distant metastasis significantly predict survival, and that patients who undergo resection for the recurrent disease have better survival than others.

Angiosarcoma has generally poor survival among Asian patients; though chemotherapy can be effective, it has been underused in the last few decades.

Aldoxorubicin yielded significantly better progression-free survival over investigator’s choice of various chemotherapy options in patients with relapsed or refractory leiomyosarcoma and liposarcoma, according to updated results of a phase III trial.
In this slide show we highlight some of the top news on sarcoma in 2016, including the first frontline FDA approval in 40 years, and studies on imaging in Ewing sarcoma, maintenance chemotherapy in osteosarcoma, and more.

A case study found that a patient with an inflammatory myofibroblastic tumor and a chromoplectic TPM3-ALK rearrangement that may be involved in tumorigenesis had a strong response to the ALK inhibitor ceritinib.

The use of a metronomic chemotherapy approach did not improve over standard chemotherapy in patients with high-grade, non-metastatic, operable osteosarcoma of the extremities.
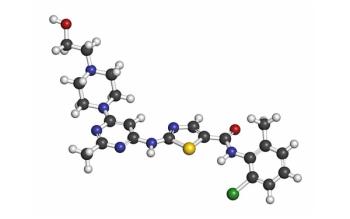
A phase II trial found that the multikinase inhibitor regorafenib has clinical activity and offers improved progression-free survival in certain types of advanced soft-tissue sarcoma.

The FDA granted accelerated approval to olaratumab (Lartruvo) in combination with doxorubicin for the treatment of soft-tissue sarcomas that is not amenable to curative treatment with radiotherapy or with surgery and with a histologic subtype treatable with anthracycline-containing regimens.

A trial of five rare sarcoma subtypes found that though dasatinib failed to achieve progression-free survival goals, more than half of patients with certain subtypes did have reasonably good survival outcomes.

In this Medical News Minute, developed exclusively for Cancer Network, Dr. Bobby Lazzara discusses a recent case report of a 1.7-million-year-old osteosarcoma found in an extinct human lineage.

The addition of palifosfamide to doxorubicin failed to improve survival in a phase III trial of patients with metastatic soft-tissue sarcoma.

Functional imaging using FDG-positron emission tomography (FDG-PET) was able to predict response to treatment in Ewing sarcoma patients, and was superior to other anatomic imaging criteria.

Alisertib yielded promising progression-free survival in advanced/metastatic soft-tissue sarcoma patients, though it did not meet its primary response rate endpoint.

A comprehensive genomic analysis of more than a thousand sarcoma patients found that about half had putatively pathogenic variations in either known or novel cancer genes.
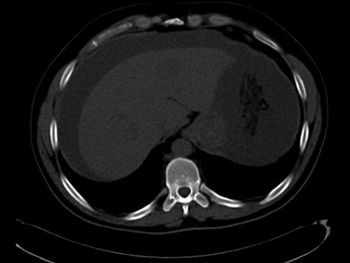
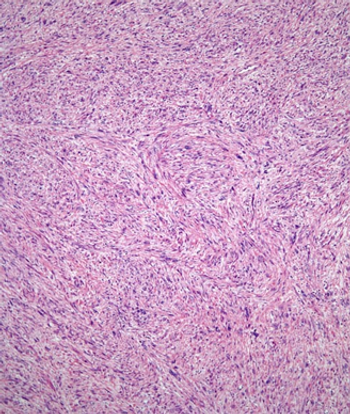
A 37-year-old Lebanese male with no significant past medical history initially presented with an increase in abdominal girth over a few weeks with worsening shortness of breath, nausea, and intermittent vomiting.

Survivors of fusion-negative sarcomas have a higher risk of developing a second malignant neoplasm than those who had fusion-positive sarcomas.

A phase I trial of selinexor found the drug was reasonably well tolerated and showed some activity in patients with advanced soft-tissue or bone sarcoma with progressive disease.

Zoledronate in combination with chemotherapy failed to improve outcomes over chemotherapy alone in patients with osteosarcoma.

Three single-nucleotide polymorphisms were identified that are significantly associated with OS in two separate cohorts of pediatric Ewing sarcoma patients.

A phase II trial showed that the tyrosine kinase inhibitor anlotinib has promising efficacy across a variety of subtypes of advanced refractory soft-tissue sarcoma.

A combination of the endoglin antibody TRC105 and pazopanib shows promising activity in patients with advanced soft-tissue sarcoma, particularly angiosarcoma.

Combined therapy with gemcitabine and pazopanib appears to be a viable treatment option for patients with soft-tissue sarcomas refractory to anthracycline or ifosfamide.