
The FDA has granted a priority review to olaratumab, in combination with doxorubicin, for the treatment of soft-tissue sarcoma.

Your AI-Trained Oncology Knowledge Connection!


The FDA has granted a priority review to olaratumab, in combination with doxorubicin, for the treatment of soft-tissue sarcoma.

Older soft-tissue sarcoma patients undergoing surgery derive greater benefit from radiotherapy than younger patients, according to a surprising analysis of more than 15,000 individuals.

While continuing to warn against use of laparoscopic power morcellators for the removal of uterus or uterine fibroids in most women, the FDA is allowing the marketing of a containment system for use with certain power morcellators to isolate tissue not suspected to be cancerous.

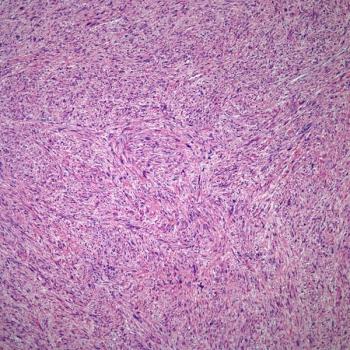
The tyrosine kinase inhibitor pazopanib appeared to have differing effects among different histologic subtypes of soft-tissue sarcoma, according to a new study conducted in Japan.

An analysis of randomized controlled trials in soft-tissue sarcoma over 40 years found that progression-free survival and response rate are reasonably well correlated with overall survival, and are thus acceptable surrogates to use.

A novel high-throughput screening assay was used to identify a number of compounds that could potentially offer therapeutic benefit in Ewing sarcoma.

A new study validated a prognostic nomogram for retroperitoneal sarcoma using a large, external cohort. The nomogram incorporates six variables, and provided strong concordance with observed disease-free and overall survival.

A phase I trial found that panobinostat combined with epirubicin is well tolerated and could offer benefit in patients with refractory sarcoma.

The FDA has granted orphan drug designation for the novel agent known as TRC105, in development by Tracon Pharmaceuticals, for the treatment of soft-tissue sarcoma.

The US Food and Drug Administration announced the approval of eribulin (Halaven) for the treatment of unresectable, metastatic liposarcoma in patients who have received prior chemotherapy with an anthracycline.

The aim of this review is to discuss current neoadjuvant treatment options for soft-tissue sarcomas.

Improvements in neoadjuvant therapy for soft-tissue sarcomas will require the development of more efficacious systemic therapies and, if possible, the performance of histology-specific, prospective, randomized clinical trials to advance the field.

The FDA granted orphan drug designation for a developmental agent known as GPX-150, an analog of doxorubicin currently being tested for use in advanced or metastatic soft-tissue sarcoma.

A phase II trial of dasatinib found that the drug did not produce strong clinical benefit in most types of advanced sarcoma, though it may have activity in undifferentiated pleomorphic sarcoma.

The presence of a TP53 mutation was associated with improved survival in patients with advanced soft-tissue sarcoma who were treated with VEGFR inhibition.

The developer of evofosfamide announced that two phase III trials of the agent in advanced soft-tissue sarcoma and in advanced pancreatic cancer did not meet their primary endpoints.

Imatinib had no impact on failure-free or overall survival in patients with gastrointestinal stromal tumor, but it did have an effect on relapse-free survival.

A treatment strategy including dose intensification with interval compression, use of the most active agents available, and the use of irinotecan as a radiation sensitizer led to a promising event-free survival rate in certain patients with metastatic rhabdomyosarcoma.

The FDA announced the approval of trabectedin (Yondelis) for the treatment of liposarcoma and leiomyosarcoma that is either unresectable or has metastasized.

The US Food and Drug Administration has granted a Priority Review designation to eribulin for the treatment of inoperable soft-tissue sarcoma.

Vascular reconstruction increases morbidity in sarcoma patients undergoing resection vs those without vascular procedures, but oncologic outcomes are similar.
Trabectedin was found to offer superior disease control to dacarbazine in patients with advanced liposarcoma and leiomyosarcoma.

Preoperative chemotherapy, both with or without concurrent radiotherapy, is feasible among patients with localized, high-risk soft-tissue sarcoma, according to a new phase III trial.

Adding bevacizumab to paclitaxel did not improve outcomes in a phase II trial of patients with angiosarcoma.

A retrospective study was used to develop nomograms predictive of both metastasis-free and overall survival for patients with nonmetastatic osteosarcoma.