Brentuximab vedotin led to unprecedented progression-free survival for patients with classical Hodgkin lymphoma.

Your AI-Trained Oncology Knowledge Connection!

Brentuximab vedotin led to unprecedented progression-free survival for patients with classical Hodgkin lymphoma.

A reduction in splenomegaly was observed when the combination of pelabresib plus ruxolitinib was used to treat patients with myelofibrosis.

Ponatinib remains a safe treatment for patients with chronic-phase chronic myeloid leukemia.

The benefit-risk profile of asciminib may change the chronic myeloid leukemia treatment paradigm, according to Jorge E. Cortes, MD.

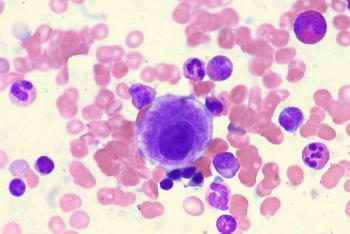
Experts from Mayo Clinic and The University of Texas MD Anderson Cancer Center discuss results from multiple myeloma trials presented at the 2023 American Society of Clinical Oncology Annual Meeting and how they may apply to clinical practice.

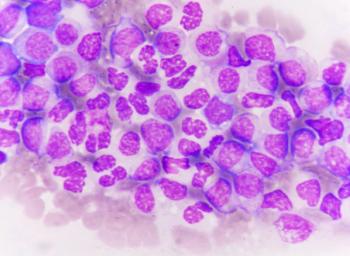
Gregory W. Roloff, MD, indicates that brexucabtagene autoleucel did not yield significant positive findings in patients with relapsed/refractory B-cell acute lymphoblastic leukemia who were MRD positive.

The education of patients on identifying and reporting adverse effects is a critical part of effective toxicity management.

One role of a physician assistant is to help patients understand their treatment and the results they’re presented with.

Adverse effect management is a concern for clinicians when administering follicular lymphoma treatment, and the use of targeted pathways may help mitigate them.
Zanubrutinib and acalabrutinib produce similar safety profiles in the treatment of patients with relapsed/refractory chronic lymphocytic leukemia in the phase 3 ASCEND and APLINE trials.

The responses to epcoritamab plus rituximab/lenalidomide for patients with relapsed/refractory follicular lymphoma appear comparable between those with and without disease progression within 24 months of first-line chemotherapy in the phase 1/2 EPCORE NHL-2 trial.
Treatment with lisocabtagene maraleucel correlates with a reduction in CD19-positive cells in responders and patients with stable disease among those with relapsed or refractory chronic lymphocytic leukemia or small lymphocytic lymphoma in the phase 1/2 TRANSCEND CLL 004 trial.
Axicabtagene ciloleucel produces a higher median overall survival vs high-dose therapy plus autologous stem cell transplant among patients with relapsed or refractory large B-cell lymphoma in the phase 3 ZUMA-7 trial.
Ciltacabtagene autoleucel may become a new standard of care for patients with lenalidomide-refractory myeloma after first relapse, according to an expert from the Medical College of Wisconsin in Milwaukee.
GCF012F may show promising activity in relapsed and refractory multiple myeloma, according to an expert from Shanghai Chang Zheng Hospital.

For the pooled analysis, investigators evaluated the efficacy and safety of bispecific antibody elranatamab in patients with relapsed/refractory multiple myeloma enrolled in 1 of the 4 MagnetisMM trials who received at least 1 proteasome inhibitor, 1 immunomodulatory drug, 1 anti-CD38 monoclonal antibody, and 1 BCMA-directed ADC and/or CAR T-cell therapy.

SWOG S1826 is an open-label trial that enrolled patients with newly diagnosed stage III or IV classical Hodgkin lymphoma who were randomly assigned to receive either nivolumab/AVD or brentuximab vedotin/AVD.

Numerous patients with heavily pretreated relapsed/refractory multiple myeloma responded following treatment with talquetamab and daratumumab.
Investigators report an increased objective response rate when linvoseltamab is given to patients with relapsed/refractory multiple myeloma.
A phase 1 trial continued to show positive responses when PHE885 was used in patients with relapsed/refractory multiple myeloma.
Results from the phase 1b RedirecTT-1 study show acceptable efficacy and safety when teclistamab plus talquetamab was given to patients with relapsed/refractory multiple myeloma.

An expert from Vanderbilt University Medical Center says that patients with relapsed/refractory multiple myeloma may be able to live a normal life following response to salvage treatment with bispecific monoclonal antibodies.
A real-world population of patients with relapsed/refractory B-cell acute lymphoblastic leukemia are reported to have had a high rate of complete remissions following treatment with brexucabtagene autoleucel.
Obecatagene autoleucel also appears to result in a high rate of minimal residual disease negativity in a population of patients with relapsed/refractory B-cell acute lymphoblastic leukemia.

Patients with highly transfusion dependent, relapsed/refractory myelodysplastic syndrome appear to have long-lasting transfusion independence and increased hemoglobin following treatment with imetelstat.
Luspatercept may lead to a paradigm shift in the treatment of patients with lower-risk myelodysplastic syndrome, according to an expert from The University of Texas MD Anderson Cancer Center.
Sustained improvements in leukemia outcomes in low- and middle-income countries are feasible with cross border programs, according to an expert from the University of California, San Diego.

Elotuzumab, lenalidomide, high-dose melphalan, as well as umbilical cord blood–derived natural killer cells and autologous stem cell transplant demonstrated tolerability and improved transplant outcomes for high-risk multiple myeloma.

Saad Z. Usmani, MD, MBA, FACP, spoke about the safety profile of standard triplet therapy with or without elotuzumab for patients with newly diagnosed, high-risk multiple myeloma in the phase 3 SWOG 1211 trial and how results of this trial may be used in future datasets to inform treatment in this setting.
C. Ola Landgren, MD, PhD, discusses progression-free survival data from the phase 3 DETERMINATION trial examining lenalidomide, bortezomib, and dexamethasone with or without autologous stem cell transplant plus continuous lenalidomide maintenance in patients with newly diagnosed multiple myeloma.