
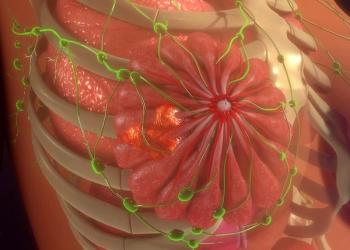
Heather Zinkin, MD, states that reflexology improved pain from chemotherapy-induced neuropathy in patients undergoing radiotherapy for breast cancer.

Your AI-Trained Oncology Knowledge Connection!


Heather Zinkin, MD, states that reflexology improved pain from chemotherapy-induced neuropathy in patients undergoing radiotherapy for breast cancer.

A prospective trial may help affirm ctDNA as a non-invasive option of predicting responses to radiotherapy among those with gynecologic cancers.

Interest in novel therapies to improve outcomes initiated an investigation of the use of immunotherapy in early-stage non-small cell lung cancer.

The agency places a partial clinical hold on the phase 3 PRESERVE-003 trial due to varying results between the squamous and nonsquamous NSCLC cohorts.

Neil M. Iyengar, MD, highlighted the most important data in breast cancer to come from 2024 ESMO.
A panel of expert pharmacists provides their perspectives on gene therapy agents such as exagamglogene autotemcel in the management of sickle cell disease.

Investigators are assessing the feasibility, safety, and efficacy of MTX110 for patients with recurrent glioblastoma as part of the phase 1 MAGIC-1 study.

ctDNA reductions or clearance also appeared to correlate with a decrease in disease burden during the pre-boost phase of radiotherapy.

Offering certain radiotherapy modalities based on disease burden may play a role in the outcomes of those with ES-SCLC, according to James Ninia, MD.

Investigators evaluated ctDNA as a potentially noninvasive method to predict response to radiotherapy among those with gynecologic malignancies.

Data from the phase 3 SPOTLIGHT trial and the phase 3 GLOW trial supported the approval of zolbetuximab plus chemotherapy in this indication.

Adolescents and young adults with cancer more commonly experience financial toxicity and unmet social needs.
Updated findings from RAMP 201 show that avutometinib/defactinib is generally well tolerated among those with low-grade serous ovarian cancer.

Those with pathogenic variants had a higher likelihood of communicating with clinicians and family members about test results.

Study findings reveal that patients with breast cancer reported overall improvement in their experience when receiving reflexology plus radiotherapy.

Patients undergoing radiotherapy for breast cancer were offered 15-minute nurse-led reflexology sessions to increase energy and reduce stress and pain.
Raymond B. Mailhot, MD, MPH, discussed how radiation therapy can impact education and survivorship for pediatric survivors of brain tumors.
Phase 3 data show that nivolumab/AVD may also reduce long-term toxicities vs brentuximab vedotin/AVD in advanced Hodgkin lymphoma.
Bin Gui, MD, discussed how ultra-hypofractionated radiotherapy may be a convenient treatment option for elderly patients with early breast cancer.

Review data demonstrated a variation in opioid prescriptions for cancer-related pain between oncology providers and pain management providers.

While cisplatin was in shortage, clinicians were forced to prescribe costlier alternatives for patients with head and neck cancer.
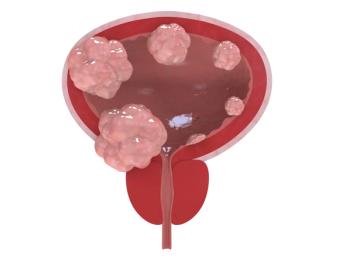
The decision is backed by robust efficacy data from the phase 3 ENVISION trial, evaluating UGN-102 in patients with non-muscle invasive bladder cancer.

Data from the phase 2 SAVANNAH trial may support savolitinib as a new treatment option following standard-of-care osimertinib in EGFR-mutated NSCLC.

Ginger J. Gardner, MD, FACOG, walked through the strides of gynecologic cancer research and emphasized the efforts that still need to be accomplished.
Significant results from a retrospective analysis of brain tumor survivor academic performance after radiotherapy emerged despite small sampling size.

Support for the approval comes from phase 3 LUNAR study findings indicating TTFields significantly prolonged OS compared with standard of care alone.

Developers plan to submit a supplemental NDA for this combination as a first-line maintenance therapy for ES-SCLC in the first half of 2025.

Findings may help providers and patients with head and neck cancer consider whether to proceed with radiotherapy modalities, such as proton therapy or IMRT.

Subgroup data indicate a positive efficacy trend for TG4001 plus avelumab among patients with cervical cancer.
Raymond B. Mailhot, MD, MPH, discussed methods for comparing academic performances of patients following radiation therapy with healthy control groups.