
Panelists discuss how the CARTITUDE-1 trial was designed to evaluate cell therapy in relapsed/refractory multiple myeloma and the importance of long-term follow-up in understanding efficacy and safety.

Your AI-Trained Oncology Knowledge Connection!


Panelists discuss how the CARTITUDE-1 trial was designed to evaluate cell therapy in relapsed/refractory multiple myeloma and the importance of long-term follow-up in understanding efficacy and safety.

Taletrectinib showed improved efficacy in patients with ROS1-positive non–small cell lung cancer who were treatment-naïve.

“It’s a drug that I’m very comfortable with, and it is a drug I’ll likely use primarily in the first-line setting,” stated Jorge Nieva, MD, on taletrectinib in non–small cell lung cancer.

Panelists discuss how both amivantamab plus lazertinib and osimertinib-based regimens show good central nervous system activity for patients with baseline brain metastases, with treatment choice influenced more by patient-specific factors like bleeding risk and anticoagulation contraindications than by CNS efficacy differences.

Panelists discuss how the MARIPOSA study demonstrated significant progression-free survival and overall survival (OS) benefits with amivantamab plus lazertinib vs osimertinib monotherapy, with mature overall survival data showing a 25% improvement in survival outcomes.

Those being treated for peritoneal carcinomatosis may not have to experience the complication rates or prolonged recovery associated with surgical options.

For patients with peritoneal carcinomatosis, integrating PIPAC into a treatment regimen does not interrupt their systemic therapy.

Panelists discuss the debate on optimal timing for initiating therapies in lower-risk myelodysplastic syndromes, balancing early intervention to improve quality of life and prevent complications against a conservative approach favoring treatment initiation upon transfusion dependency or symptom onset.
Panelists emphasized that for a patient with metastatic HER2-positive breast cancer and active brain metastases, selecting a treatment with proven intracranial activity is critical, while carefully considering prior therapy tolerability, radiation history, and the balance between treatment efficacy and patient convenience to optimize both disease control and quality of life.

Panelists discuss findings from the IMerge phase 3 trial of imetelstat in lower-risk myelodysplastic syndromes, emphasizing its impact on transfusion independence and fatigue improvement, and advocating for a sequential, patient-centered treatment approach to enhance quality of life and long-term outcomes.
Panelists discussed a complex case of a 47-year-old woman with metastatic HER2-positive breast cancer, emphasizing the importance of continuous systemic therapy despite treatment interruptions, the critical role of multidisciplinary care for central nervous system involvement, and the need to balance efficacy with quality of life as patients navigate prolonged disease courses and evolving treatment strategies.
Panelists discuss the adoption of 4-drug regimens—including a CD38 monoclonal antibody—as the standard frontline therapy for patients with transplant-eligible multiple myeloma, emphasizing tailored modifications based on age and frailty, and evolving maintenance strategies that incorporate daratumumab to deepen and sustain responses post-transplant.
Panelists discuss how immune cell–associated neurotoxicity syndrome data mirrors cytokine release syndrome patterns, with 70% of patients experiencing no neurotoxicity, only 5% to 7% developing grade 3 or higher events, and most toxicities occurring early and resolving within 1 week, further supporting arguments for modified monitoring approaches.

Counseling Patients on ADC Side Effects Patient education is a cornerstone of successful ADC treatment. When introducing ADCs, providers focus on transparency—discussing the most common side effects upfront and reinforcing that many are reversible with dose holds or modifications. Eye toxicities and lung-related side effects like pneumonitis often cause anxiety. Clear communication and reassurance that these can be managed effectively help build trust. Educational materials and follow-up calls ensure patients feel supported and informed. Ultimately, the goal is to empower patients to report symptoms early and remain engaged in their care. ADC therapy offers significant clinical benefit, and with proactive management, patients can achieve extended survival and maintain their quality of life throughout treatment.

Panelists discuss the real-world comparison of ciltacabtagene autoleucel (cilta-cel) and idecabtagene vicleucel (ide-cel) chimeric antigen receptor (CAR) T-cell therapies for multiple myeloma, highlighting cilta-cel’s superior efficacy but higher toxicity and emphasizing the importance of tailoring treatment decisions to individual patient factors such as disease stage, health status, and personal preferences.

Panelists discuss the transformative impact of chimeric antigen receptor (CAR) T-cell therapy on treating relapsed/refractory multiple myeloma (R/R MM) in real-world settings, emphasizing improved patient outcomes, the expanding role of real-world evidence, and the nuanced decision-making required in selecting among newly approved, highly effective immunotherapies.
Panelists discuss the manageable safety profile of 4-drug regimens in patients with transplant-eligible multiple myeloma, highlighting dose modifications such as weekly bortezomib and dexamethasone tapering to reduce adverse effects, alongside vigilant infection monitoring to optimize tolerability and quality of life.
Panelists discuss how data from over 1500 patients receiving liso-cel shows consistent cytokine release syndrome (CRS) outcomes between clinical trials and real-world settings, with most CRS events occurring within the first 2 weeks and late-onset events being rare and manageable, supporting potential changes to monitoring protocols.

Panelists discuss how managing ADC-related ocular toxicity requires vigilance through slit-lamp exams and visual acuity testing, with early intervention including treatment holds or dose reductions being essential to prevent long-term damage, while emphasizing the need for collaborative decision-making between oncologists and ophthalmologists to balance cancer control with reversible side effects and maintain patient quality of life.

According to Benjamin J. Golas, MD, PIPAC could be used as a bridging therapy before surgical debulking or between subsequent large surgical operations.

Samuel Rosner, MD, discusses how the treatment landscape for EGFR-mutated non–small cell lung cancer has evolved from first-generation targeted therapies to osimertinib as the current standard of care, while exploring emerging options like fourth-generation tyrosine kinase inhibitors, antibody-drug conjugates, and bispecific therapies to overcome resistance mechanisms.

Panelists discuss how the evolution of FDA approvals for multiple myeloma therapies reflects rapid innovation and increasing effectiveness, particularly with cell-based treatments.

Panelists discuss how advancements in treatment options, including chimeric antigen receptor (CAR) T-cell therapy, bispecific antibodies, and antibody-drug conjugates, are shaping the current multiple myeloma landscape.
Panelists discuss how the extended median follow-up data from the MonumenTAL-1 trial demonstrate that Q2 weekly dosing of talquetamab shows superior progression-free survival (11.2 vs 7.5 months), duration of response (19.5 vs 7.5 months), and overall survival compared with weekly dosing, with particularly encouraging efficacy in high-risk cytogenetics and older patients while maintaining a manageable safety profile.
Panelists discuss how bispecific antibodies have evolved in relapsed/refractory myeloma treatment, highlighting recent data developments, the importance of NCCN guideline updates, including prophylactic tocilizumab recommendations, and strategies for improving toxicity management and community practice implementation.
Panelists discuss how cytokine release syndrome can be managed through early intervention with tocilizumab and steroids, and emphasize the importance of patient and staff education for safe outpatient administration.
![“If you have a [patient in the] fourth or fifth line, [JNJ-5322] could be a valid drug of choice,” said Rakesh Popat, BSc, MBBS, MRCP, FRCPath, PhD.](https://cdn.sanity.io/images/0vv8moc6/cancernetwork/267879fc15a40ec8d3ed04d8ee9c1f044b49ee89-2990x1692.png?w=350&fit=crop&auto=format)
“If you have a [patient in the] fourth or fifth line, [JNJ-5322] could be a valid drug of choice,” said Rakesh Popat, MBBS, PhD, MRCP, FRCPath.
Panelists discuss how talquetamab shows a more favorable safety profile with significantly lower high-grade infection rates compared with B-cell maturation antigen (BCMA)–directed bispecifics, although a new cerebellar toxicity signal requires monitoring.

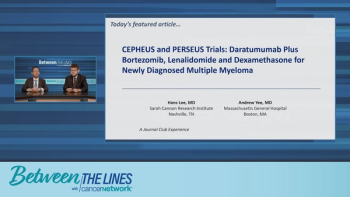
Earlier treatment with daratumumab may be better tolerated for patients with pretreated MRD-negative multiple myeloma.
The trispecific antibody JNJ-5322 demonstrated superior efficacy vs approved agents in multiple myeloma in results shared at the EHA 2025 Congress.