Heather McArthur, MD, spoke about the use of CDK4/6 inhibitors in the adjuvant setting for patients with HR+/HER2– breast cancer.

Your AI-Trained Oncology Knowledge Connection!

Heather McArthur, MD, spoke about the use of CDK4/6 inhibitors in the adjuvant setting for patients with HR+/HER2– breast cancer.

“Developments that take high-dimensional data and come up with interpretable insights…are going to play an increasing role,” says Smita Krishnaswamy, PhD.
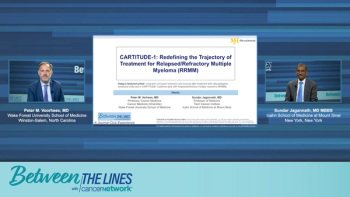
Panelists discuss how the efficacy outcomes from CARTITUDE-1, including a substantial progression-free survival (PFS) benefit, highlight the transformative impact of deep, sustained minimal residual disease (MRD)-negative responses.

Panelists discuss how comprehensive patient education about expected adverse effects, combined with prophylactic measures including dexamethasone premedication and dermatologic support, helps patients successfully tolerate amivantamab plus lazertinib therapy while maintaining treatment adherence.

Panelists discuss how to operationalize talquetamab dosing in community settings by addressing the main challenges of infection risk and skin toxicity through patient education, proactive monitoring protocols, and careful patient selection, with early community experience showing manageable toxicity rates and the importance of setting proper expectations about skin and nail changes as markers of drug activity rather than concerning adverse effects.

Panelists discuss how the emerging trispecific antibody (targeting both T cells and natural killer [NK] cells) has generated significant excitement with its unprecedented 100% overall response rate in B-cell maturation antigen (BCMA)–exposed patients, while incorporating lessons learned from earlier bispecifics such as starting with Q4 weekly dosing and built-in tocilizumab prophylaxis, although they acknowledge this breakthrough may completely reshape treatment sequencing strategies and create new challenges in determining optimal therapy combinations.

Panelists discuss how real-world experience with amivantamab plus lazertinib has shown remarkable responses consistent with trial data, including effectiveness in challenging cases like leptomeningeal disease, with manageable adverse effects when proper prophylactic measures and patient education are implemented.
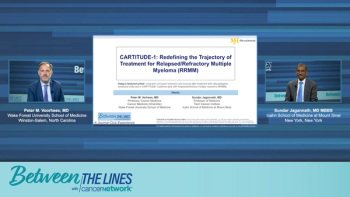
Panelists discuss how CARTITUDE-1 addressed an unmet need by targeting late-line, refractory myeloma patients with a fixed dose of chimeric antigen receptor (CAR) T-cell therapy for potential accelerated approval.

An expert discusses how comprehensive genomic profiling will continue growing as an essential component of personalized cancer care, expanding into serial testing for resistance monitoring, tumor burden tracking, and potentially earlier-stage cancers as targeted therapies prove effective beyond advanced disease.

An expert discusses how education about the clinical impact of genomic testing, understanding of targeted therapies, turnaround times, and team-based approaches are essential to bridge the gap in routine comprehensive genomic profiling adoption.

An expert discusses how comprehensive genomic profiling panels that include relevant targets, resistance markers, and clonal hematopoiesis information have proven most useful, along with technologies that can detect fusion events, point mutations, and copy number variations for serial monitoring over time.

An expert discusses how molecular profiling has become essential for most solid tumor cancers, particularly in lung cancer, where both tissue- and plasma-based testing using next-generation sequencing help identify actionable genomic targets and monitor resistance patterns.

An expert discusses how molecular profiling has become essential for most solid tumor cancers, particularly in lung cancer, where both tissue- and plasma-based testing using next-generation sequencing helps identify actionable genomic targets and monitor resistance patterns.
Panelists discuss how improving CAR T accessibility through reduced monitoring requirements could strengthen its position against bispecific antibodies in treatment decision-making, emphasizing that access considerations should only influence therapy choice when efficacy and safety are comparable, not when CAR T demonstrates superior outcomes.
Panelists highlighted the impressive central nervous system activity of trastuzumab deruxtecan demonstrated in the DX12 trial, underscoring the need for multidisciplinary collaboration to optimize treatment of brain metastases and reduce reliance on whole-brain radiation, while acknowledging ongoing challenges in sequencing and patient selection amid evolving therapies.
Panelists discuss how successful outpatient bispecific therapy requires robust infrastructure, including 24-hour monitoring capabilities, emergency department coordination, and liberal use of supportive medications.
Panelists agreed that beyond third-line therapy for HER2-positive metastatic breast cancer, treatment becomes highly individualized—often described as the “wild West”—with options including various monoclonal antibodies, tyrosine kinase inhibitors, chemotherapy, and emerging agents; decisions are largely based on prior toxicities, patient preferences, and disease biology, with clinical trials playing a crucial role in offering promising new therapies that may outperform standard care.

Panelists discuss the sequencing of therapies in lower-risk myelodysplastic syndromes, debating whether to initiate treatment with erythropoiesis-stimulating agents due to cost and patient variability or with luspatercept for its superior efficacy and potential disease-modifying effects, while highlighting ongoing trials exploring combined or sequential strategies.
Panelists highlighted that the HER2CLIMB study showed adding tucatinib to trastuzumab and capecitabine provides a meaningful progression-free survival benefit in HER2-positive metastatic breast cancer with brain metastases, balancing improved intracranial control against manageable toxicities like diarrhea and hand-foot syndrome, and underscored the importance of patient education and dose management to maintain adherence and quality of life.
Panelists discuss how findings from a Mayo Clinic retrospective study demonstrate the feasibility and safety of outpatient step-up dosing for talquetamab, with minimal hospitalizations required.

Panelists discuss treatment strategies for lower-risk myelodysplastic syndromes guided by serum erythropoietin (EPO) levels, weighing the reduced efficacy of erythropoiesis-stimulating agents at higher EPO levels against newer therapies’ benefits and challenges, and emphasizing personalized sequencing based on patient and disease characteristics.

Panelists discuss the critical role of sequencing B-cell maturation antigen (BCMA)-targeted therapies in multiple myeloma, emphasizing that administering chimeric antigen receptor (CAR) T-cell therapy before bispecific antibodies leads to better outcomes, while real-world evidence and emerging guidelines increasingly inform strategic decisions based on treatment timing, disease urgency, and patient-specific factors.
Panelists discuss updated American Society of Clinical Oncology (ASCO) data confirming that daratumumab-based quadruplet therapy (Dara-VRD) significantly improves progression-free survival (PFS) and sustains minimal residual disease (MRD) negativity in patients with newly diagnosed transplant-eligible multiple myeloma, reducing early relapses and reinforcing this regimen as the evolving standard of care with potential for unprecedented long-term outcomes.
Panelists discuss the Perseus study, which compared daratumumab-based quadruplet therapy (Dara-VRD) with VRD alone in patients with newly diagnosed, transplant-eligible multiple myeloma, highlighting its focus on a generally fit population and demonstrating improved progression-free survival and deeper responses with the 4-drug regimen, while noting some limitations in applicability to patients with significant comorbidities.

Panelists discuss the emerging real-world use of talquetamab as a bridging therapy before chimeric antigen receptor (CAR) T-cell treatment in patients with advanced multiple myeloma, highlighting its ability to rapidly reduce tumor burden and improve CAR T outcomes despite unique toxicities and emphasizing how clinician-driven innovation is shaping practice ahead of clinical trial data.

The CHALLENGE trial in CRC studied structured exercise and demonstrated a DFS benefit comparable to or exceeding oxaliplatin chemotherapy.

According to Jorge Nieva, MD, there are a multitude of things that can be explored to enhance the treatment landscape for lung cancer.

Panelists discuss how the availability of multiple B-cell maturation antigen (BCMA) bispecific agents (with linvoseltamab approved in Europe and other agents in development) creates beneficial competition that could drive down costs and provide more treatment options, while acknowledging that safety and efficacy profiles appear comparable across agents, making accessibility and convenience key differentiating factors for patient care.
Panelists discuss how the baseline characteristics of CARTITUDE-1 participants underscore the trial’s focus on patients with heavily pretreated and refractory disease.

Panelists discuss how recent long-term follow-up data for teclistamab and elranatamab reaffirm their effectiveness in relapsed/refractory multiple myeloma (R/R MM) with no new safety signals, while emphasizing that direct comparisons between B-cell maturation antigen (BCMA) bispecifics may not be fair due to evolving mitigation strategies, improved supportive care practices, and different study conditions including the impact of COVID-19 on early trials.