
Once a patient-specific dose is determined, an all-oral combination of revumenib plus decitabine/cedazuridine and venetoclax may be “very good” in AML.

Your AI-Trained Oncology Knowledge Connection!


Once a patient-specific dose is determined, an all-oral combination of revumenib plus decitabine/cedazuridine and venetoclax may be “very good” in AML.

Patients with lung cancer who achieve a complete response with neoadjuvant therapy may not experience additional benefit with adjuvant immunotherapy.

Numerous trials have displayed the evolution of EGFR inhibition alone or with chemotherapy/radiation in the EGFR-mutated lung cancer space.
Demonstrates that longer amivantamab exposure further reduces the emergence of MET and EGFR mutations.

Although high grade adverse effects are infrequent among patients undergoing treatment for SCLC, CRS and ICANS may occur in higher frequencies.
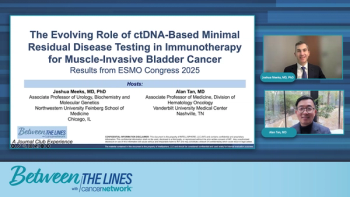
The experts conclude this program by discussing future biomarker-guided approaches in bladder cancer treatment.

Co-hosts Kristie L. Kahl and Andrew Svonavec highlight what to look forward to at the 67th Annual ASH Meeting in Orlando.

Misako Nagasaka, MD, PhD, summarizes the key takeaways: proactive AE management, CNS vigilance, and strategic sequencing as hallmarks of modern care for EGFR-mutant NSCLC.

Based on a patient’s SCLC subtype, and Schlafen 11 status, patients will be randomly assigned to receive durvalumab alone or with a targeted therapy in the S2409 PRISM trial.

The discussion underscores the role of multidisciplinary coordination in maintaining adherence, quality of life, and long-term therapeutic benefit.

Daniel Peters, MD, aims to reduce the toxicity associated with AML treatments while also improving therapeutic outcomes.

Findings from numerous clinical trials vindicating the addition of immunotherapy to first-line chemotherapy in SCLC have emerged over the past several years.

Patients with AML will experience different toxicities based on the treatment they receive, whether it is intensive chemotherapy or targeted therapy.

A younger patient with AML who is more fit may be eligible for different treatments than an older patient with chronic medical conditions.

Breast cancer care providers make it a goal to manage the adverse effects that patients with breast cancer experience to minimize the burden of treatment.

Social workers and case managers may have access to institutional- or hospital-level grants that can reduce financial toxicity for patients undergoing cancer therapy.

Genetic backgrounds and ancestry may hold clues for better understanding pancreatic cancer, which may subsequently mitigate different disparities.

Factors like genetic mutations and smoking may represent red flags in pancreatic cancer detection, said Jose G. Trevino, II, MD, FACS.

Thomas Hope, MD, believes that an NRC initiative to update infiltration guidelines may organically address concerns that H.R. 2541 outlines.
Insurance and distance to a tertiary cancer center were 2 barriers to receiving high-quality breast cancer care, according to Rachel Greenup, MD, MPH.

Experts debate when to introduce chemotherapy, how to manage its cumulative toxicity, and how to de-escalate maintenance regimens.

The panel explores integrating molecular data to guide therapy selection and optimize sequencing strategies after resistance emerges.

Thomas Hope, MD, had not observed an adverse effect attributable to an infiltration across more than a decade of administering nuclear agents at UCSF.
The panelists investigate emerging molecular testing technologies, focusing on whole genome sequencing and advanced profiling techniques.
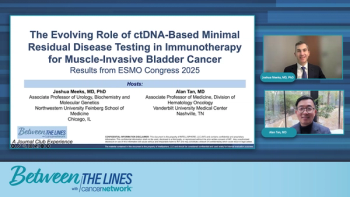
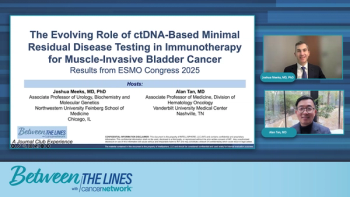
The discussion centers on the Imvigor011 trial, comparing its ctDNA-guided intervention approach to prostate cancer monitoring. Dr. Meeks and Dr. Tan explore how this prospective study could transform adjuvant therapy strategies in muscle-invasive bladder cancer (MIBC).
![According to John Henson, MD, “What we need are better treatments to control the [brain] tumor once it’s detected.”](https://cdn.sanity.io/images/0vv8moc6/cancernetwork/e0d29c38bb732429ae370e4ef7d1829a10c96446-2992x1684.png?w=350&fit=crop&auto=format)
According to John Henson, MD, “What we need are better treatments to control the [brain] tumor once it’s detected.”

First-degree relatives of patients who passed away from pancreatic cancer should be genetically tested to identify their risk for the disease.
Panelists discuss how evolving MRD-driven and immune-based therapies are shaping a personalized future for NDMM management.
Panelists discuss how infection prevention and selective IVIG use are critical for maintaining safety during NDMM combination therapy.

Surgery and radiation chemotherapy can affect immunotherapy’s ability to target tumor cells in the nervous system, according to John Henson, MD.