Oncology NEWS International
- Oncology NEWS International Vol 10 No 9
- Volume 10
- Issue 9
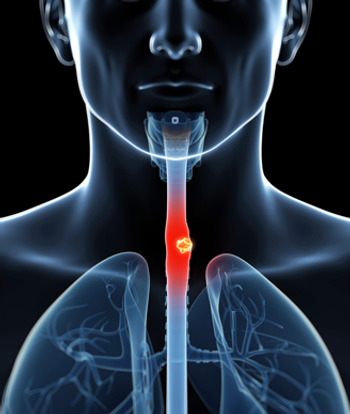
Irinotecan, Cisplatin, and Radiotherapy Tested in Esophageal Cancer
NEW YORK-Esophageal cancer, though relatively rare in the United States, is deadly, with a 90% mortality for patients treated with conventional therapy. David H. Ilson, MD, PhD, assistant attending physician at Memorial Sloan-Kettering Cancer Center in New York City, described new multimodal attempts to improve these outcomes.
NEW YORKEsophageal cancer, though relatively rare in the United States, is deadly, with a 90% mortality for patients treated with conventional therapy. David H. Ilson, MD, PhD, assistant attending physician at Memorial Sloan-Kettering Cancer Center in New York City, described new multimodal attempts to improve these outcomes.
A US Intergroup study (INT-113) showed no advantage to adding five cycles of 5-fluorouracil (5-FU) plus cisplatin (Platinol) before surgery in treating locally advanced disease. Dr. Ilson said that a recent, larger trial from the United Kingdom reported an advantage to two cycles of 5-FU/cisplatin prior to surgery, but the median and 2-year survival were no better than survival with surgery alone in the Intergroup trial. "Most of us have focused on concurrent radiation and chemotherapy, with or without surgery, as the strategy to pursue in future studies," he said.
Trials of preoperative chemoradiation have reported pathologic complete responses in 20% to 40% of patients, with 5-year disease-free survivals of 25% to 35%. "These regimens can have substantial toxicity, particularly with infusional 5-FU and cisplatin. Because of the poor survival and the toxicity of currently available therapy we need to look at new agents," Dr. Ilson said.
Irinotecan is Radiosensitizer
Irinotecan (Camptosar) is attractive in this regard because cell lines and xenografts show that it is a radiosensitizer. Dr. Ilson said that the mechanism of radiosensitization might be increased recruitment of cells into the G2/M phase, the most radiosensitive part of the cell cycle. Irinotecan, a topoisomerase inhibitor, also might enhance lethal double-strand DNA breaks.
Phase I lung cancer trials done in Japan suggested that combining irinotecan, cisplatin, and radiotherapy was feasible. Recent studies of irinotecan-based therapy in esophageal and gastric cancers reported a single-agent response rate of 15% and combination response rates of about 50% to 60%.
A phase I trial of weekly irinotecan (65 mg/m²) and cisplatin (30 mg/m²) on a 4-week-on, 2-week-off schedule conducted at Memorial Sloan-Kettering Cancer Center caused minimal toxicity and was associated with responses in esophageal and gastrointestinal (GI) cancers.
"We then took the regimen to a phase II trial in 35 patients with a response rate of 57%," Dr. Ilson said. "This was one of the most active regimens we screened in metastatic disease. We also saw dysphagia relief that was remarkable. Ninety percent of patients with dysphagia had relief with chemotherapy." The combination was well tolerated. Half of patients had grade 3 or 4 myelosuppression, but most cases were grade 3. Only 11% of patients had grade 3 diarrhea.
Adding Other Therapies
The investigators thought that adding other therapies to this regimen was feasible. Dr. Ilson’s group is now conducting a phase I study of irinotecan/cisplatin plus concurrent radiation in patients with locally advanced esophageal cancer. "We give 6 weeks of induction chemotherapy with irinotecan/platinum on a 2-week-on, 1-week-off schedule to relieve dysphagia. This is followed by 6 weeks of combined chemoradiation, again 2-weeks-on, 1-week-off. During the radiation the cisplatin dose is fixed at 30 mg/m² and irinotecan is being dose escalated. We’re now up to 80 mg/m²," Dr. Ilson said.
Eighteen patients have been enrolled, most with stage III disease. Fifteen patients are evaluable for toxicity. "We have seen essentially no grade 3-4 toxicity on this regimen. We had one patient with reversible pneumonitis, but we have seen no grade 3-4 esophagitis. We have seen minimal hematologic toxicity using this 2-week-on, 1-week-off schedule, and even at the 65 mg/m2 dose level of irinotecan, the median ANC nadir was 2.2. Dose-limiting myelosuppression was seen only at the 80 mg/m2 dose of irinotecan," Dr. Ilson said.
Although this is a phase I trial, complete responses have been seen in 5 of 13 patients treated (38%). Three of these were pathologic complete responses. Tumors were downstaged in 8 of 10 patients (80%).
Posttreatment Finding
A surprising posttreatment finding was that asymptomatic pulmonary emboli appeared on post-treatment computed tomography (CT) scans in 3 of 15 patients. "In only one of three patients was there a coincident deep venous thrombosis (DVT), and this patient was probably progressing on therapy," Dr. Ilson said. "We don’t have an explanation for these pulmonary emboli." Increased pulmonary emboli or DVT were not observed in prior phase I and II trials that included more than 100 patients with metastatic disease. Dr. Ilson has now added Coumadin prophylaxis during the course of chemoradiation to the regimen.
Weekly 1-hour paclitaxel is now being added to the cisplatin/irinotecan/radiotherapy regimen, and a future trial is planned to include SU-5416.
Articles in this issue
over 24 years ago
Avon Launches ‘Kiss Goodbye to Breast Cancer’ Campaignover 24 years ago
Occult Tumor Cells in Marrow Predict Breast Cancer Survivalover 24 years ago
No Long-Term Advantage for Complete Response to Neoadjuvant Chemo/RTover 24 years ago
New Agents Tested with 5-FU in Rectal Cancerover 24 years ago
Anticonvulsants Can Alter Irinotecan Metabolismover 24 years ago
Thalidomide Appears Effective in Early-Stage Myelomaover 24 years ago
New ‘Goals for Pain Relief’ Scale Proves Reliable in Pilot Studyover 24 years ago
GVAX Autologous Vaccine Shows Activity in Lung CancerNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.