Oncology NEWS International
- Oncology NEWS International Vol 9 No 4
- Volume 9
- Issue 4
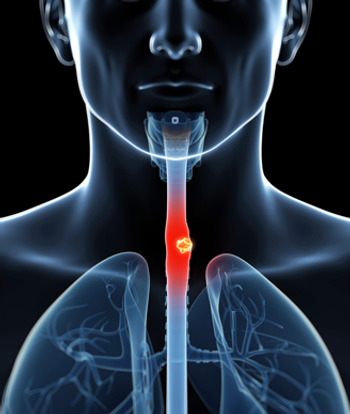
New Approach for Early Cancer Detection in Barrett’s Esophagus
PHOENIX-A more aggressive endoscopic biopsy protocol detected more early cancers in Barrett’s esophageal tissue than the standard protocol. Moreover, two separate studies have begun to identify specific genetic markers that may allow physicians to stratify patients with Barrett’s esophagus according to their risk for cancer progression.
PHOENIXA more aggressive endoscopic biopsy protocol detected more early cancers in Barretts esophageal tissue than the standard protocol. Moreover, two separate studies have begun to identify specific genetic markers that may allow physicians to stratify patients with Barretts esophagus according to their risk for cancer progression.
These studies, presented at the 64th Annual Scientific Meeting of the American College of Gastroenterology and conducted at the Fred Hutchinson Cancer Research Center, Seattle, begin to address some of the controversies surrounding the management of patients with Barretts esophagus.
Historically, biopsies have been taken from all four walls of the esophagus at 2-cm intervals, but we had concerns of missing early cancer, said Douglas S. Levine, MD, principal investigator for the endoscopic study, and currently the chief medical officer at AstraZeneca, LP. By shifting to a more aggressive 1-cm protocol, in addition to sampling all visible lesions, we intended to decrease diagnostic error, he said.
This study involved 123 patients with Barretts esophagus and high-grade dysplasia who had no obvious cancer on endoscopy. After the initial diagnosis of high-grade dysplasia, the first two follow-ups were done within 6 months. When two successive procedures confirmed high-grade dysplasia without cancer, follow-up was extended to not more than 6 months.
Of the 123 patients studied, 45 had microscopically confirmed esophageal adenocarcinoma; 29% were detected with the first endoscopy, and 71% were detected during follow-up, Dr. Levine said. Notably, among two thirds of the patients in whom cancer was detected, the endoscopic appearance of the Barretts mucosa was unremarkable, illustrating the importance of taking a sufficient number of biopsies.
Because high-grade dysplasia indicates a high risk for cancer, the researchers also derived models to gauge the cancer detection rates of various endoscopic biopsy protocols. These models showed that in patients without visible lesions, biopsies done every 2 cm would have missed 50% of the cancers detected with the 1-cm approach (P < .0001). And if only the visible lesions were biopsied, roughly 66% of the cancers would have been overlooked.
Endoscopists need to consider these data if they wish to offer continued biopsy surveillance to patients with high-grade dysplasia in Barretts esophagus, Dr. Levine said. If surgical intervention is not undertaken for high-grade dysplasia, endoscopic biopsy surveillance should be carried out using a 1-cm, four-quadrant biopsy protocol at closely timed intervals.
Chromosomal Abnormalities
While this aggressive biopsy protocol is effective, it was not designed to dictate changes in clinical practice. And high-grade dysplasia alone many not be the best predictor of the development of cancer in Barretts esophagus.
In this regard, two separate studies investigated the genetic profiles of tissue from Barretts segments to begin to identify specific chromosomal lesions that might act as markers for risk stratification and, possibly, disease progression.
The researchers studied the Barretts mutation profiles from 213 cell populations obtained from 61 patients and purified by flow cytometry . One study analyzed the mutation patterns for the p53 tumor suppressor gene (n = 58), while the other analyzed the loss of heterozygosity (LOH) (n = 60) observed for the p53 and/or the p16 tumor suppressor genes. Biopsy samples were taken at 2-cm intervals.
Of the 58 high-grade dysplasia patients evaluated for p53 mutations, 29 (50%) had mutations in this gene within their Barretts tissue, said Brian J. Reid, MD, PhD, head of the Program in Gastrointestinal Oncology and lead investigator of both studies. None of these patients had detectable cancer, Dr. Reid said. Moreover, the expansion pattern of a single mutant clone was observed to encompass entire sections (up to 9 cm) of Barretts tissue, and individual patients were also seen to possess multiple p53 mutant clones.
The second study involved the p16 and p53 genes, which are encoded on chromosomes 9p21 and 17p13, respectively. The inactivation of these loci through LOH is the most commonly occurring event in esophageal adenocarcinoma; inactivation of 9p is observed in 75% of cases and inactivation of 17p in 95% of cases.
The study showed that the Barretts esophagus tissue of patients with high-grade dysplasia contains a mosaic of mutant clones with varying abnormal chromosome complements and differing levels of LOH: 9p alone, 17p alone, or both, Dr. Reid said.
He pointed out that when both abnormalities are detectable in the same patient, 9p LOH tends to occur before 17p LOH, implying a possible temporal relationship between these mutations.
Importantly, we found that the proportion of patients with LOH at both genetic loci was comparable to the proportion of patients with high-grade dysplasia in the Seattle Barretts Esophagus Study who progressed to cancer within 5 years, Dr. Reid said. He noted that further prospective study is needed to verify these initial findings.
Thus, the combined use of systematic endoscopic evaluation and genetic marker analyses appears to hold promise for identifying Barretts patients at risk for cancer. However, endoscopic ablation or surgical resection must be carefully evaluated in light of the clonal distribution patterns observed within Barretts tissue. Leaving residual clones behind after such interventions could result in redeveloped high-grade dysplasia and possibly cancer, Dr. Reid concluded.
Articles in this issue
almost 26 years ago
NCCN Physicians Get an ‘A’ for Guidelines Concordancealmost 26 years ago
Marketing Prostate Cancer Screening Services to Womenalmost 26 years ago
Physicians Bring End-of-Life Program Back to Communitiesalmost 26 years ago
Radiolabeled Tositumomab for Transformed Low-Grade NHLalmost 26 years ago
Topotecan Doses Individualized in Neuroblastomaalmost 26 years ago
Encouraging Results for Gene Therapy in CLLalmost 26 years ago
Number of US Cancer Deaths Remained Steady in 1997almost 26 years ago
Director Tells How NCI Will Spend Budget Increasesalmost 26 years ago
IOM Report on Minority Research Praises NCI Effortsalmost 26 years ago
Breast MRI Changes Management of Occult Primary CancersNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.