Oncology NEWS International
- Oncology NEWS International Vol 19 No 8
- Volume 19
- Issue 8
Sonography better to monitor small testicular lesions
There is a lack of scientific evidence about the risk of testicular cancer associated with testicular lesions, but the conventional treatment approach has been immediate surgical removal because of the possibility of malignancy. A more conservative approach has served one Canadian institution well when it comes to active surveillance of small, incidentally discovered testicular masses.
There is a lack of scientific evidence about the risk of testicular cancer associated with testicular lesions, but the conventional treatment approach has been immediate surgical removal because of the possibility of malignancy. A more conservative approach has served one Canadian institution well when it comes to active surveillance of small, incidentally discovered testicular masses.
For nearly a decade, ultrasound (US) surveillance has been offered to men as an alternative to surgical treatment at the University of Toronto, and, thus far, the approach has spared many patients from unnecessary surgery.
The majority of the men present at the Mount Sinai Hospital Fertility Clinic for a fertility evaluation. During these tests, nonpalpable testicular masses less than 1 cm have been detected incidentally.
Paul J. Toren, MD, and colleagues reviewed their experience using an ultrasound surveillance strategy between 2001 and 2008. Their series of patients is the largest to date to demonstrate the benign nature of most small, nonpalpable, incidental testicular masses, Dr. Toren said.
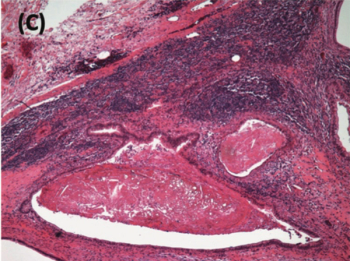
The series included 45 men who had one or more hypoechoic, nonpalpable intratesticular masses less than 1 cm in diameter. Infertility was the reason for referral in 39 men. On serum analysis, 16 subjects showed evidence of azoospermia, 16 men had oligospermia, and seven had normospermia. Semen analysis was not available in six men.
"Surgery should be limited to men whose lesional growth points to a malignancy and men with positive tumor markers." - Paul J. Toren, MD
The mean follow-up in the study from the first to the last ultrasound was 253 days. Patients were also examined by a urologist before or after the ultrasound examination to confirm there were no palpable lesions.
Thirty-eight patients had serial ultrasound surveillance only, with a mean yearly lesional growth of 0.5 mm.
Overall, eight patients underwent surgery. Three had immediate surgery and five underwent surgery after a period of initial ultrasound surveillance. Surgery was indicated in two patients because of interval growth; in the other six, the decision for surgery was made by the patient.
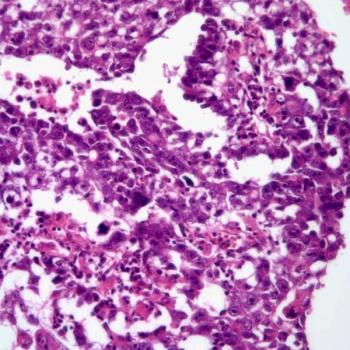
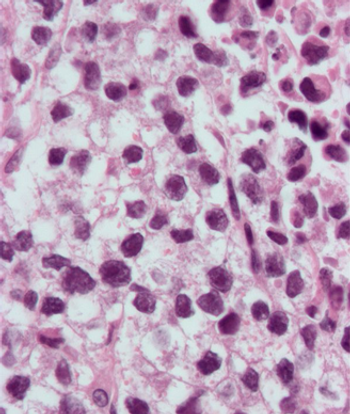
Only one patient had radical orchiectomy for pure seminoma following an interval growth from 3 mm to 6 mm at ultrasound at three months. He has had no recurrent disease to date, Dr. Toren reported. The other seven masses excised by partial orchiectomy were benign (2010 American Urological Association abstract 1928).
The authors concluded that most small, incidental, nonpalpable testicular masses could be safely followed with serial ultrasound and did not show significant growth requiring surgery.
"Our findings support a conservative approach involving active surveillance with ultrasound monitoring in men who have an incidental finding of a small testicular mass on ultrasound," said Dr. Toren, a urology resident.
While his group does not have formal data on the appropriate time for follow-up, the men initially seen at the fertility clinic are routinely followed with repeat serial ultrasound for at least six months.
He recommended that most men with a small nonpalpable lesion on their initial testicular ultrasound have a second ultrasound one month later and then again every three months for at least six months. Surgery should be limited to men whose lesional growth points to a malignancy and men with positive tumor markers, Dr. Toren said.
Study pinpoints factors that sway testicular cancer survival
Single men, ages 40 and up, are more likely to have unfavorable outcomes after a diagnosis of testicular cancer, according to a population-based study of 27,948 patients.
Researchers based in Rochester, New York, and Oslo looked at cumulative 10-year testicular cancer–specific mortality as reported to the SEER database from 1978 to 2006. The men (15 years and older) had histologically confirmed seminoma (16,007) or nonseminoma (11,887). Socioeconomic status was calculated, and the parameters included in the analysis were extent of disease, postorchiectomy surgery (RPLND-recorded since 1998), radiotherapy, marital status, and race. Data on chemotherapeutic status were not available. Overall survival of five-year testicular cancer survivors was compared with rates for men in the general population.
The authors reported that the cumulative 10-year mortality for seminoma patients diagnosed at age 40 or older was 2.3% vs 1.4% for those under age 40. For nonseminoma patients, the 10-year mortality rate was 6.1% for those under age 40 and 9.1% for those above.
Age and socioeconomic status were significantly associated with unfavorable mortality for nonseminoma patients along with being single, being nonwhite, having metastatic disease, and having no record of postorchiectomy treatment. For seminoma patients, the same variables, except race and socioeconomic status, were significant. After three decades of follow-up, small significant differences in overall survival were observed between five-year testicular cancer survivors, who displayed lower overall survival rates than the general population (ASCO 2010 abstract 4578).
Articles in this issue
over 15 years ago
Who's Newsover 15 years ago
FDA Panel Says No More Avastin in Breast Cancerover 15 years ago
Cell-signaling pathway may be new Rx target ER+ breast cancerover 15 years ago
Ohio cancer center breaks ground on $1 billion additionover 15 years ago
Imaging experts debate link between CT scans, cancer riskNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.
Related Content