
As part of our MBCC coverage we discuss MRI screening for breast cancer in patients who carry a BRCA mutation or have a first-degree relative who is a BRCA carrier.

Your AI-Trained Oncology Knowledge Connection!


As part of our MBCC coverage we discuss MRI screening for breast cancer in patients who carry a BRCA mutation or have a first-degree relative who is a BRCA carrier.

Economic factors, including household income, and racial disparities both play a role in the adherence to hormonal therapy in breast cancer patients.

The addition of bevacizumab to endocrine therapy did not prolong survival in postmenopausal women with advanced HER2-negative, HR–positive breast cancer.
An inhibitor of osteoclast formation can stop the proliferation of dormant tumor cells that in some breast cancer survivors turn into bone metastases.

The FDA has approved the CDK4/6 inhibitor palbociclib (Ibrance) for the treatment of postmenopausal women with metastatic breast cancer.

The benefit of hypofractionated radiotherapy for women receiving breast-conserving therapy for early-stage breast cancer is becoming more apparent.

Many women with breast cancer do not understand the details of their tumor characteristics or how they relate to specific treatment options, according to a new study.
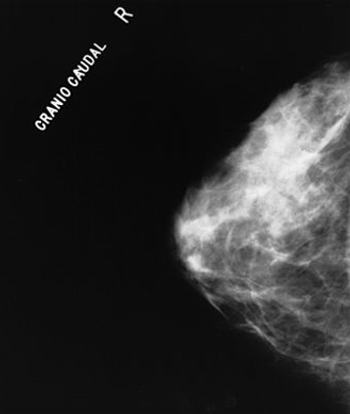
Adding molecular breast imaging to mammography resulted in a fourfold increase in invasive breast cancer detection rates in women with dense breasts.

There are still questions to be answered about the use of osteoclast inhibitors in the care of patients with breast cancer. The optimal duration and dosing schedule and how to improve treatment compliance are important issues to address.

Bisphosphonates have played an important role in the treatment of breast cancer, mainly in patients with bone metastasis, by reducing the risk of fracture, spinal cord compression, and hypercalcemia.

We know that bisphosphonates prevent or delay skeletal-related events in breast cancer metastatic to bone, prevent or treat bone loss in patients receiving adjuvant aromatase inhibitor therapy, and decrease bone recurrences and breast cancer–related deaths when used in the adjuvant setting in postmenopausal women with early-stage breast cancer.

Bisphosphonates or the monoclonal antibody denosumab, have the potential to profoundly affect the entire metastatic process, not just the growth of bone metastases.

Two recently published studies suggest that PIK3CA mutations cannot be used as a predictive biomarker to guide therapy in HER2-positive breast cancer.

Adding an MRI to a mammogram improved the sensitivity of breast cancer screening in women 50 years of age or older who are BRCA mutation carriers.

Results of the MARIANNE trial found that HER2-positive breast cancer patients treated with T-DM1 had similar survival to those on the current standard of care.

A retrospective cohort study of women treated for early-stage breast cancer has confirmed rising trends in the proportion of patients who undergo mastectomy.

An analysis of a large number of women suggested that those who use bisphosphonates, a bone medication used to treat osteoporosis and other bone loss diseases, have a reduced risk of endometrial cancer.

A large trial showed that treatment-emergent vasomotor and/or joint symptoms do not correlate with any improvement in recurrence-free survival in postmenopausal breast cancer patients treated with aromatase inhibitors.

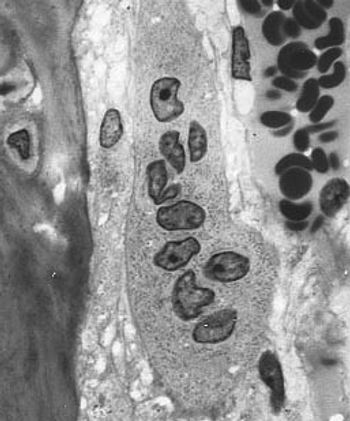
This review will focus on properties of cancer stem cells; will compare and contrast the cancer stem cell model with the clonal evolution model of tumorigenesis; will discuss the role of cancer stem cells in the development of resistance to chemotherapy; and will review the therapeutic implications and challenges of targeting cancer stem cells, with an assessment of the potential such an approach holds for improving outcomes for patients with cancer.

Treatments that target cancer stem cells have been proposed as alternatives to current cancer therapies. However, the clonal evolution model suggests that multiple tumor cell populations may need to be targeted for these treatments to be successful.

Accelerated partial breast irradiation was shown to be just as effective and safe as whole breast irradiation in early-stage breast cancer patients.
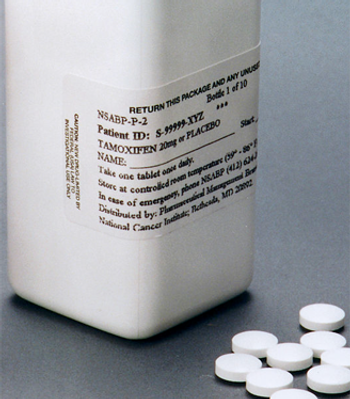
Tamoxifen given to women at high risk for breast cancer lowered the rate of estrogen receptor (ER)-positive breast cancer diagnosis in the IBIS-I trial.

Fulvestrant improved overall survival compared with anastrozole, among women with treatment-naive, advanced, hormone receptor-positive breast cancer.

Data from the Women’s Intervention Nutrition Study found a reduction in dietary fat intake resulted in lower death rates in ER- and PR-negative breast cancer.

The PD-1 inhibitor pembrolizumab showed activity and had an acceptable safety profile in heavily pretreated metastatic triple-negative breast cancer patients.