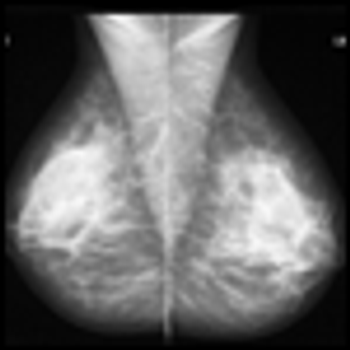
The number of patients in the U.S. treated with radiation has increased at an average annual rate of about 7% between 2007 and 2009, according to the “2010 Radiation Therapy Market Summary Report” by IMV. Breast, prostate, and lung cancers continue to be the cancer types treated most frequently with radiation.