
The FDA approved enzalutamide, a once-daily oral therapy for men with metastatic castration-resistant prostate cancer that has either spread to other organs or recurred, despite prior surgical or medical treatment.

Your AI-Trained Oncology Knowledge Connection!


The FDA approved enzalutamide, a once-daily oral therapy for men with metastatic castration-resistant prostate cancer that has either spread to other organs or recurred, despite prior surgical or medical treatment.
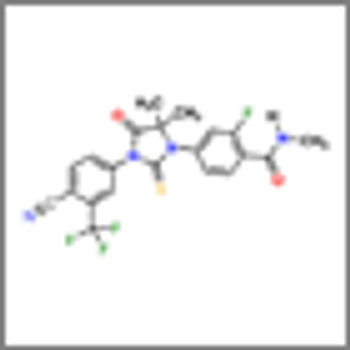
Results of the phase III AFFIRM trial shows that enzalutamide (MDV3100) significantly prolonged survival of men with metastatic castration-resistant prostate cancer after chemotherapy

We discuss the current controversies in prostate cancer-PSA screening and approaches to initial treatment for men diagnosed with the disease.

According to a study in the journal Cancer, without the use of PSA screening the number of men presenting with cases of metastatic prostate cancer would be three times greater than the actual number observed today.

The results of the 12-year PIVOT trial shows men with early-stage prostate cancer who had a radical prostatectomy did no better than those actively monitored without surgery.

How should oncologists advise patients about the best surgical approach to use to treat their prostate cancer? Quite simply, it is the surgeon, not the approach. The self-fulfilling prophecy about surgery is that the best surgeons tend to do the most surgeries, so an easy metric is volume.

In summary, both RALP and ORP are excellent operations in experienced hands. They are also technically difficult to perform consistently well, so in my view, surgeons should attempt to master the operation they perform rather than hastily switching to robotic surgery, unless they have an opportunity for significant mentorship and surgical volume.

We fervently hope that all surgeons will participate in a comparative outcomes project for the purpose of quality improvement. However, today we will settle for one, we hope, skilled surgeon, open or robotic.

Over the last decade, robotic-assisted laparoscopic prostatectomy (RALP) has rapidly gained in popularity, primarily for three reasons: the enthusiasm of surgeons keen to try something new, medical marketing, and patients’ desire to avoid side effects from surgery.

There is no question that the robot has leveled the playing field. It has allowed more surgeons to offer patients a minimally invasive approach. In terms of perioperative outcomes, there is clear evidence showing shorter hospital stays, less blood loss, lower complication rates, and shorter convalescence with robotic-assisted laparoscopic prostatectomy.
A new noninvasive blood test for prostate cancer detection won the approval of the FDA last month. The manufacturer believes the test will provide better detection and a decrease in costs.

This review by Aneja et al provides an excellent discussion of prostate external beam hypofractionated radiation therapy and its potential benefits and pitfalls.

In this issue of ONCOLOGY, Aneja and colleagues explore the beneficial aspects of the use of hypofractionated radiotherapy in the treatment of adenocarcinoma of the prostate.

Given that prostate cancer is the most common non-cutaneous cancer among men in the Western world, its treatment is of great medical and public significance.

Researchers reported results of an international phase III trial showing that intermittent hormonal therapy is less effective than continuous therapy in prostate cancer with minimal disease.
Results from a randomized phase II study show that 6 months of treatment with abiraterone (Zytiga), in addition to the hormone therapy leuprolide before prostatectomy, resulted in complete response and near-complete response in one-third of men with high-risk prostate cancer.

The underlying cost debate surrounding the issue of whether or not to recommend prostate cancer screening is based on the idea that if you use healthcare resources in one area, they’re being diverted from another area by nature of their being a limited pool of funding.
Two experts discuss newly available and upcoming treatment options, such as abiraterone and MDV3100, for patients with castration-resistant prostate cancer.

Radium-223 is a promising agent that represents a new class of alpha pharmaceuticals that gets down to the site of bony metastases. The limited side-effect profile potentially allows for repeat administration to increase durability of pain control, and for its use in combination with novel biologic and chemotherapeutic agents.

One would hope that survival data from at least one more phase III or phase IV clinical trial will convincingly show a prolongation of survival due to treatment with Alpharadin. This will not be inexpensive therapy.

This article will present current information about alpha-pharmaceuticals, a new class of targeted cancer therapy for the treatment of patients with CRPC and bone metastases. It will review preclinical and clinical studies of the experimental radiopharmaceutical radium-223 chloride (Alpharadin).

Use of neoadjuvant metformin prior to radical prostatectomy helped to reduce metabolic effects and slow the growth rate of cancer in a single-center phase II study conducted among men with confirmed prostate cancer.

Rationale for prostate cancer screening continues to be debated as an update to a large European trial reconfirms a reduction in death rates from prostate cancer in men who are screened for the disease. The study, however, found no significant difference in overall mortality between the two arms of the trial.
The new drug, MDV3100, extended overall survival by 4.8 months (P < .001) and reduced the risk for death by 37% as compared to placebo in men with castration-resistant prostate cancer who had progressed after treatment with docetaxel.

Screening is always an issue that generates a great deal of emotion, as recently seen with the controversies surrounding mammography and prostate-specific antigen (PSA) testing.