
At this year’s ASCO GU Cancers Symposium, several high-impact and potentially practice-changing abstracts were presented during the prostate cancer session.

Your AI-Trained Oncology Knowledge Connection!


At this year’s ASCO GU Cancers Symposium, several high-impact and potentially practice-changing abstracts were presented during the prostate cancer session.
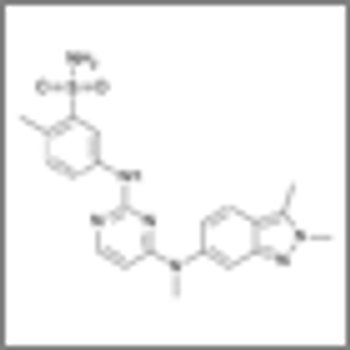
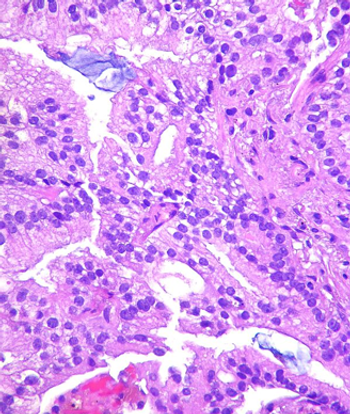
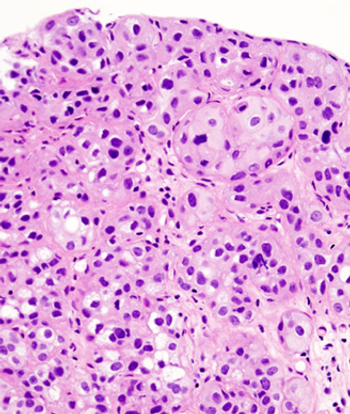
Phase II study results found that half of patients with relapsed or refractory urothelial carcinoma responded to treatment with pazopanib and paclitaxel.

In this interview we discuss the changing landscape of systemic therapies for the treatment of bladder cancer.

As part of our coverage of the ASCO GU Cancers Symposium, we discuss decision-making in the management of patients with early-stage prostate cancer.

The 4Kscore blood test has been shown to accurately detect the presence of high-grade prostate cancer, according to a study presented at ASCO GU.

Two clinical factors may predict PSA response to cabazitaxel in men with metastatic castration-resistant prostate cancer.
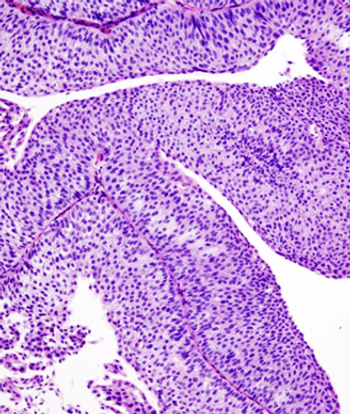
Patients with bladder cancer derived an overall survival benefit from the use of adjuvant chemotherapy compared with observation.
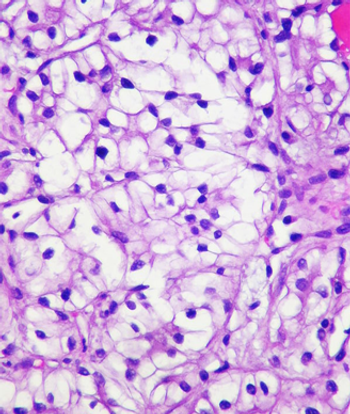
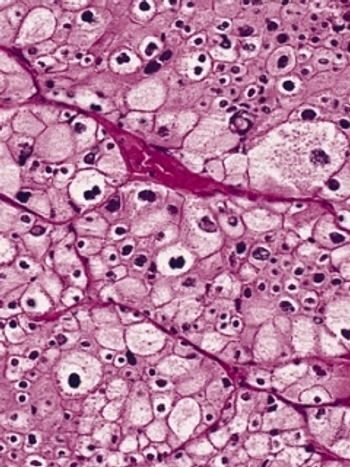
Metastatic renal cell carcinoma patients with an elevated neutrophil-to-lymphocyte ratio at baseline had inferior outcomes compared to those with a low ratio.

Intermediate-risk prostate cancer patients managed with surveillance had worse outcomes compared with low-risk prostate cancer patients managed with surveillance.

High-dose radiation therapy did not improve overall survival compared with the standard dose in stage II localized prostate cancer, but did show some benefits.
A large retrospective analysis suggests the number of patients diagnosed with intermediate- and high-risk prostate cancer has increased since 2011.
Levels of AR-V7 in metastatic castration-resistant prostate cancer patients could guide physicians to treat with either taxanes or enzalutamide/abiraterone.

Patients with a history of testicular cancer had a fivefold higher risk of developing aggressive prostate cancer when compared with those with no history of testicular cancer.

The TKI famitinib was associated with a significant PFS improvement in metastatic colorectal cancer patients, according to the results of a phase II study.
Hepatocellular carcinoma patients with baseline alpha-fetoprotein (AFP) levels greater than 400 ng/mL may derive greater benefit from second-line ramucirumab.
Combining MM-398 with 5-FU/leucovorin chemotherapy in metastatic pancreatic cancer patients resulted in improved survival compared with 5-FU/leucovorin alone.

The addition of ramucirumab to second-line FOLFIRI resulted in a delay in disease progression and improved survival in metastatic colorectal cancer patients.

Newly diagnosed metastatic colorectal cancer patients with higher vitamin D levels had better outcomes after treatment with chemotherapy and a targeted agent.

Rectal cancer patients who completed neoadjuvant therapy with a clinical complete response had similar 4-year survival rates as patients who opted for surgery.
Initial treatment with FOLFOXIRI plus bevacizumab in metastatic colorectal cancer patients improved survival over FOLFIRI and bevacizumab by more than 4 months.

In this interview we discuss prostate cancer highlights from the 2014 ASCO Genitourinary Cancers Symposium.
A new study found that induction bladder-conserving treatment was safe in patients with muscle-invasive bladder cancer who achieved only a near-complete response.

The order of the sequencing of sorafenib and sunitinib for first-line and second-line therapy did not affect progression-free and overall survival for patients with advanced renal cell carcinoma.

A recent analysis of more than 7,000 adult cancer clinical trials has found that about 20% of trials fail to complete for reasons unrelated to efficacy or adverse events of the intervention.
The use of angiotensin system inhibitors significantly improved the survival of patients with metastatic RCC who were on the drug for the treatment of hypertension, according to the results of a retrospective study presented at the ASCO GU Symposium.

Adding a treatment course of local radiotherapy to hormonal treatment in men with locally advanced or high-risk prostate cancer more than halved the 10-year and 15-year prostate-cancer–specific mortality.
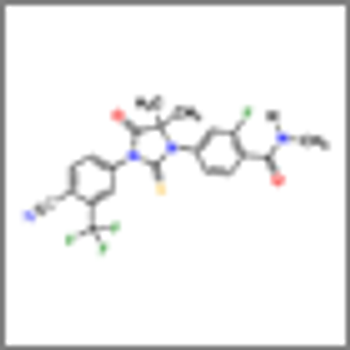
Androgen inhibition with enzalutamide significantly reduced the risk of disease progression and increased survival among men with previously untreated metastatic prostate cancer, according to the results of the phase III PREVAIL trial.

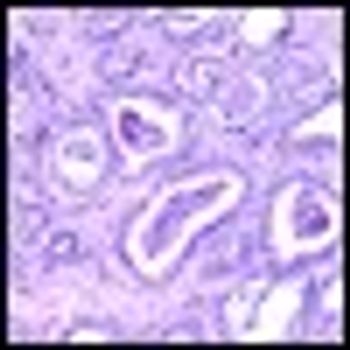
The use of adjuvant radiotherapy in patients with pT3 prostate cancer subsequent to radical prostatectomy is safe, according to 10-year follow-up results presented at the 2013 Genitourinary Cancers Symposium.

In two phase III studies-READY and VENICE-targeted agents combined with standard first-line chemotherapy failed to increase overall survival for men with metastatic castration-resistant prostate cancer.
Physicians treating men with high-risk prostate cancer can safely reduce the duration of androgen blockade given in combination with pelvic radiation from 36 months to 18 months without compromising outcomes, including survival.