
Findings from the phase 3 SUNLIGHT study highlight favorable overall survival and disease control rates with the use of bevacizumab plus trifluridine and tipiracil in metastatic colorectal cancer.

Your AI-Trained Oncology Knowledge Connection!


Findings from the phase 3 SUNLIGHT study highlight favorable overall survival and disease control rates with the use of bevacizumab plus trifluridine and tipiracil in metastatic colorectal cancer.

Novel, personalized, tumor-informed brPROPHET technology can assess molecular residual disease with greater sensitivity than other assays, according to initial data.

Patients with hepatocellular carcinoma treated from 2018 to 2021 experienced better outcomes than patients treated in the preceding decade, according to a recent study.

Molecular responders by G360 response algorithm with advanced colorectal cancer appear to have significantly lengthened time on treatment and overall survival with all regimens vs patients who did not respond.

An expert from the Mayo Clinic discusses how findings from the ongoing phase 3 MOUNTAINEER trial may enable access to tucatinib, trastuzumab, and chemotherapy in earlier lines of treatment for patients with HER2-positive metastatic colorectal cancer.
Investigators report evidence of early efficacy with SEA-CD40, chemotherapy, and pembrolizumab in patients with metastatic pancreatic ductal adenocarcinoma.

Patients with advanced biliary tract cancer experience modest clinical benefit following treatment with atezolizumab and cisplatin/gemcitabine with or without bevacizumab.
Patients diagnosed with locally advanced, hepatocellular carcinoma experience benefit in overall survival, progression-free survival, and time to disease progression following treatment with sorafenib and stereotactic body radiation therapy.

Patients with newly diagnosed, advanced biliary tract cancers do not have a statistically significant survival benefit following treatment with nab-paclitaxel plus gemcitabine and cisplatin.

A combination of liposomal irinotecan plus 5-fluorouracil, leucovorin, and oxaliplatin in the frontline yields a statistically significant survival benefit compared with nab-paclitaxel and gemcitabine in a population diagnosed with metastatic pancreatic ductal adenocarcinoma.
Patients with unresectable hepatocellular carcinoma experienced an improvement in several health-related quality of life measures following treatment with first-line tislelizumab compared with sorafenib.
Lenvatinib in combination with blank-microsphere transarterial chemembolization and sequential microwave ablation demonstrates encouraging preliminary activity in patients with hepatocellular carcinoma.
Envafolimab in combination with lenvatinib and transarterial chemoembolization demonstrated efficacy and safety among patients with unresectable hepatocellular carcinoma.

Findings from the phase 3 HIMALAYA trial indicate that durvalumab with or without tremelimumab remained efficacious regardless of the presence of anti-drug antibodies in unresectable hepatocellular carcinoma.
Findings from the phase 3 LEAP-002 study indicate that the addition of pembrolizumab to lenvatinib did not impact quality-of-life scores among patients with hepatocellular carcinoma.

Lenvatinib yields survival benefit in hepatocellular carcinoma following progression on immunotherapy.

Patients with previously untreated advanced gastric cancer, gastroesophageal junction cancer, and esophageal adenocarcinoma continue to benefit from treatment with nivolumab and chemotherapy.

Long-term survival benefit is seen in patients with treatment-naïve advanced esophageal squamous cell carcinoma who were treated with nivolumab plus chemotherapy or ipilimumab.

Investigators report benefit in patients with CLDN18.2-positive, HER2-negative locally advanced unresectable or metastatic gastric/gastroesophageal junction adenocarcinoma treated with first-line zolbetuximab and mFOLFOX6.
HER-Vaxx with standard-of-care chemotherapy yielded benefit in patients with HER2-overexpressing metastatic or advanced gastric/gastroesophaeal junction adenocarcinoma.

Pre-operative tremelimumab plus durvalumab elicited encouraging safety and activity in patients with microsatellite instability–high resectable gastric or gastroesophageal junction cancer.

The findings, according to a group of researchers, warrant the development of treatments that attack HER2-low advanced gastric cancer.

Zev A. Wainberg, MD, discusses future research efforts for the treatment of patients with advanced gastric cancer.
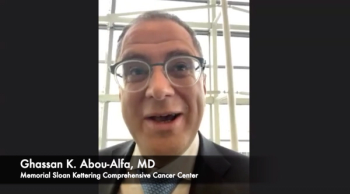
Ghassan K. Abou-Alfa, MD, detailed the evolution of treatment options for unresectable hepatocellular carcinoma prior to the phase 3 HIMALAYA study and the reasons for launching the trial.

Jun Gong, MD, hosted a Twitter takeover during the 2022 Gastrointestinal Cancers Symposium where he discussed breaking presentations in a #CNRealtimeReport.

Zev A. Wainberg, MD, spoke to the rationale for examining the efficacy of pembrolizumab alone and in combination with chemotherapy for patients with advanced gastric and gastroesophageal junction adenocarcinoma.

Patients with pretreated gastrointestinal stromal tumors who were treated with ripretinib did not reach the primary end point of progression-free survival superiority vs sunitinib in the phase 3 INTRIGUE study.

Patients with recurrent hepatocellular carcinoma after liver transplantation were treated with lenvatinib and saw promising efficacy.

The CheckMate 9X8 trial did not hit the primary end point of progression-free survival superiority with nivolumab plus standard of care vs standard of care alone in metastatic colorectal cancer.

The observational GALAXY study found that use of a ctDNA assay could help determine which patients with colorectal cancer stand to benefit the most by receipt of adjuvant chemotherapy.