
Data from the phase 3 APPLY-PNH trial show comprehensive control of intravascular and extravascular hemolysis with iptacopan in patients with paroxysmal nocturnal hemoglobinuria and persistent anemia.

Your AI-Trained Oncology Knowledge Connection!


Data from the phase 3 APPLY-PNH trial show comprehensive control of intravascular and extravascular hemolysis with iptacopan in patients with paroxysmal nocturnal hemoglobinuria and persistent anemia.
Phase 2 results showed that the investigational monoclonal antibody axatilimab elicited encouraging clinical activity and tolerability across dose levels in patients with recurrent or refractory chronic graft-vs-host disease.

Retrospective, real-world results showed that oral decitabine and cedazuridine and standard parenteral hypomethylating agents demonstrated similar levels of comorbidities and disease burden in patients with myelodysplastic syndrome.
Single-agent treatment with odronextamab continued to demonstrate encouraging clinical activity, along with a manageable safety profile, in patients with relapsed/refractory diffuse large B-cell lymphoma.

When used as a minimal residual disease (MRD)–guided treatment approach, ibrutinib (Imbruvica) combined with venetoclax (Venclexta) improved progression-free and overall survival (OS) compared with fludarabine, cyclophosphamide, and rituximab (Rituxan; FCR) in patients with treatment-naive chronic lymphocytic leukemia (CLL), as observed in the phase 3 FLAIR trial.
Dose reductions and interruptions of navitoclax plus ruxolitinib in the TRANSFORM-1 trial appear to be mostly due to thrombocytopenia, according to Naveen Pemmaraju, MD.
Older patients with hematological malignancies who received Orca-T therapy plus myeloablative chemotherapy have similar relapse-free survival rates compared with younger patients.
No patients with myelodysplastic syndrome have any grade 3 or higher acute graft-versus-host disease following treatment with Orca-T in a phase 1b study.
A virtual care platform significantly reduces hospital days for patients who are receiving CAR T-cell therapy, says Tonya Cox, BSN, RN, OCN.

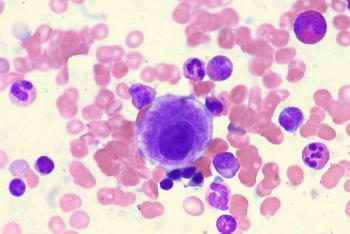
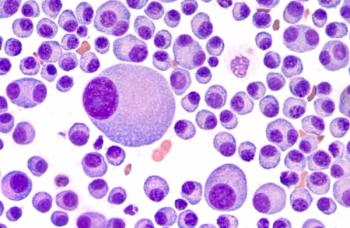
An AI algorithm was created to distinguish prefibrotic primary myelofibrosis and essential thrombocythemia from each other.

In a conversation during the 2022 American Society of Hematology Annual Meeting, an expert from the University of Texas MD Anderson Cancer Center, spoke to how treatments have improved for patients with mantle cell lymphoma.
Momelotinib continues to show benefit in reducing splenic symptoms and anemia in myelofibrosis in the second-line setting, making it a likely first treatment choice, according to an expert from the University of Texas MD Anderson Cancer Center.
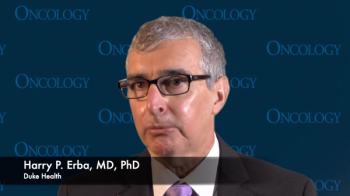
Harry P. Erba, MD, PhD, highlights key data on ziftomenib in patients with relapsed/refractory acute myeloid leukemia and its potential as part of a combination regimen.
According to the phase 3 PERSIST-1 trial and PAC203 trial, thrombocytopenia was associated with myelofibrosis treatment.

Patients with IDH1-mutant relapsed/refractory acute myeloid leukemia achieved a notable complete response rate following treatment with olutasidenib.
Patients with chronic lymphocytic leukemia or small lymphocytic lymphoma achieved promising early responses following treatment with BCB-11417 with or without zanubrutinib.

BCMA/CD19 dual-targeting FasTCAR-T Cells resulted in an overall response rate of 100% among patients with multiple myeloma, with all evaluable patients showing MRD negativity to 12 months.
Real-world data associate axicabtagene ciloleucel with temporarily worse quality of life in patients with diffuse large B cell lymphoma, transformed follicular lymphoma, or follicular lymphoma, which improves within 1-year post-infusion.

Patients with myelofibrosis and anemia who were previously treated with a JAK inhibitor experienced durable responses up to 48 weeks with momelotinib.
Treatment with induction and maintenance ibrutinib combined with chemoimmunotherapy and autologous stem cell transplant resulted in statistically significantly improved outcomes in a younger population with mantle cell lymphoma.
Those with chronic myeloid leukemia, Philadelphia chromosome-positive acute lymphoblastic leukemia, and those with CML whose tumors have a T315I mutation, were found to have improved efficacy when olverembatinib was given.

Lisocabtagene maraleucel was found to have superior efficacy in the second-line over standard of care therapy for patients with relapsed/refractory large B-cell lymphoma.

Updated findings from the phase 2 CARTITUDE-2 trial highlighted the promising efficacy of ciltacabtagene autoleucel in patients with relapsed or refractory multiple myeloma following early relapse.
Patients with with primary central nervous system lymphoma experienced prolonged progression-free survival and a reduction in risk of death following treatment with high-dose chemotherapy and autologous stem cell transplant compared with non-myeloablative chemoimmunotherapy.
Patients with B-cell malignancies intolerant to acalabrutinib appeared to derive clinically meaningful benefit from zanubrutinib.
Birtamimab treatment led to longer survival in patients with Mayo Stage IV amyloid light chain amyloidosis at 9 month follow-up.
A 3-drug regimen with post-transplant cyclophosphamide may represent a new prophylactic option for well-matched adults with graft-versus-host disease who underwent reduced-intensity transplant.

Blinatumomab plus consolidation chemotherapy produced a 58% reduction in the risk of death vs consolidation chemotherapy alone in patients with MRD-negative B-cell acute lymphoblastic leukemia.

Results from the phase 3 ALPINE trial found improved progression-free survival and overall response rate when Zanubrutinib was given to patients with chronic lymphocytic leukemia or small lymphatic leukemia vs ibrutinib.
Mosunetuzumab produced durable responses with a tolerable toxicity profile in patients with relapsed/refractory follicular lymphoma, according to an updated analysis of the phase 2 GO29781 study.