Is Aurora A kinase inhibitor alisertib superior to standard treatment protocol for peripheral T-cell lymphoma?

Your AI-Trained Oncology Knowledge Connection!

Is Aurora A kinase inhibitor alisertib superior to standard treatment protocol for peripheral T-cell lymphoma?
Cancer Network speaks with Peter Ruvolo, PhD, about his work investigating the role of microenvironments in cancer and treatment resistance.
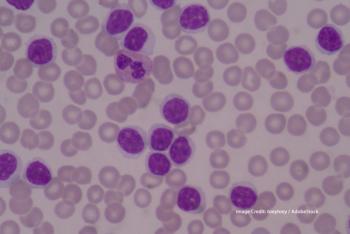
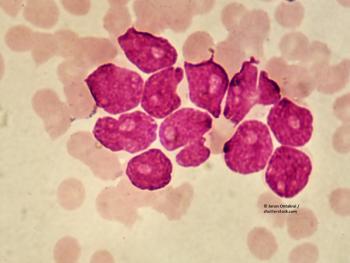
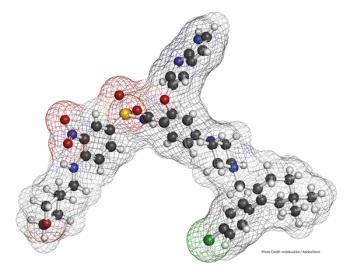
Investigators evaluated whether AZD3463 can induce apoptosis in a dose-dependent manner in a subset of AML patients.

The study, published in JAMA Oncology, examined whether treatment of 22 solid tumor types was associated with two therapy-related conditions.
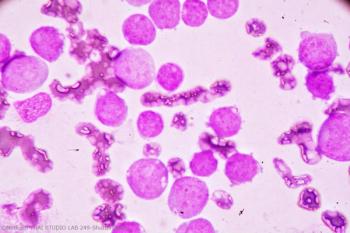
Researchers evaluated the primary mechanisms governing drug resistance and relapse in patients treated with crenolanib, an FLT3 inhibitor.

A retrospective study finds that younger mantle cell lymphoma patients may achieve longer PFS with AHCT consolidation.

Allogeneic transplantation was found not to improve overall outcome, in particular for patients who achieved MRD-negative status after induction.

Dr. Daver discusses immunotherapy approaches for patients with acute myeloid leukemia (AML), and his recent study results on the combination of azacitidine and nivolumab.

Cancer Network sat down with Dr. Naval Daver to discuss advancements and discoveries in immunotherapy for AML patients.

Guidelines for cancer screening in survivors of childhood HL may be refined based on the results of this extended follow-up study, say the researchers.
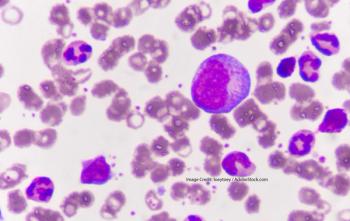
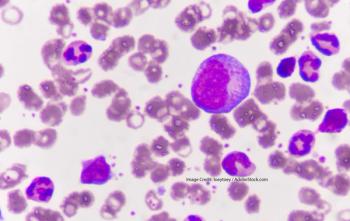
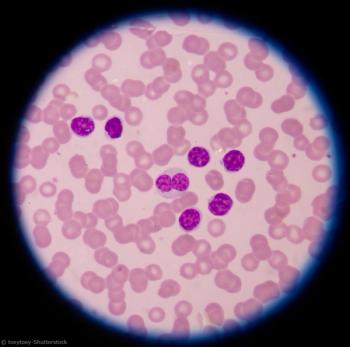
A new study published in Cancer compared ELN-2017 to ELN-2010 in terms of distinguishing prognosis in younger patients with newly diagosed AML.
Researchers reported on the impact of adding the Hedgehog pathway inhibitor glasdegib to low-dose cytarabine.

In an interview with Cancer Network, Brad S. Kahl, MD, weighs in on the top CLL research presented at ASH 2018 in San Diego.
The US Food and Drug Administration recently approved a new agent for treatment of adult patients with relapsed or refractory acute myeloid leukemia.
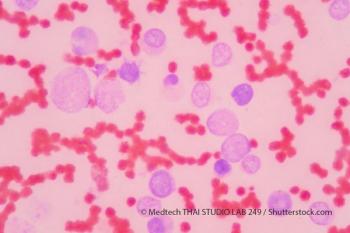
Clinicians now have a new treatment to offer elderly patients with newly diagnosed acute myeloid leukemia who have comorbidities that preclude the use of intensive chemotherapy.
A study shows sequential monitoring of the WT1 mRNA is of value for the early detection of hematologic relapse in patients with AML in remission.
A patient’s minimal residual disease status may serve as a surrogate marker for outcome in clinical trials of chronic lymphocytic leukemia in patients with comorbidities.
Azacitidine may delay or prevent relapse among patients with MRD-positive acute myeloid leukemia or myelodysplastic syndrome.
Testing patterns associated with the diagnosis and treatment of chronic lymphocytic leukemia have changed rapidly during the last decade.
The results of a follow-up analysis to the phase III MAVORIC study were presented at the ASH 2018 Annual Meeting & Exposition.
In the single-arm, multicenter, phase II part of the CAVALLI trial, the researchers analyzed the efficacy of 800-mg venetoclax plus R-CHOP in all first-line DLBCL patients.

Research presented at ASH 2018 examined whether checkpoint blockade therapy sensitizes patients with relapsed/refractory NHL to consequent treatment.
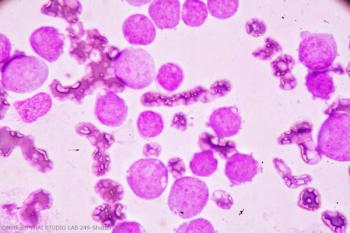
Researchers analyzed a new recurrent BCL2 mutation appearing in a cohort of patients with CLL-type progressions treated with venetoclax.

Leukemia cells show sensitivity to restriction of BCL2 and BTK with the combination of venetoclax and ibrutinib.
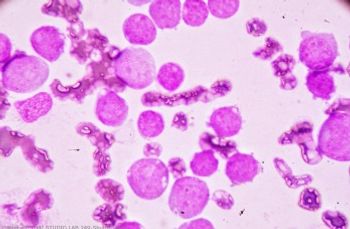
Allogeneic hematopoietic stem cell transplantation could improve outcomes of elderly patients with acute myeloid leukemia.