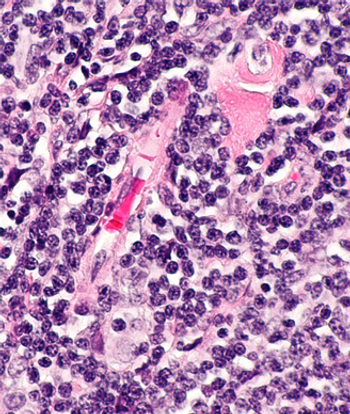
The first-in-human clinical trial for TruUCAR GC027 in relapsed or refractory T-cell acute lymphoblastic leukemia was announced by Gracell Biotechnologies.

Your AI-Trained Oncology Knowledge Connection!

The first-in-human clinical trial for TruUCAR GC027 in relapsed or refractory T-cell acute lymphoblastic leukemia was announced by Gracell Biotechnologies.
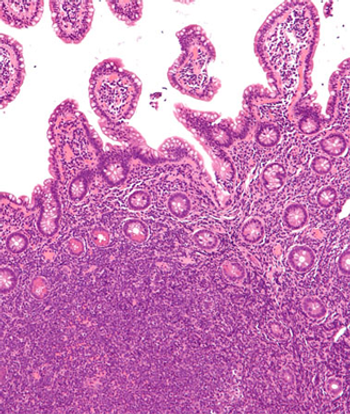
Hypercalcemia at diagnosis of diffuse large B-cell lymphoma was found to be strongly correlated with adverse prognostic factors and a short diagnosis-to-treatment interval.

The FDA granted orphan drug designation to Ascentage Pharma’s HQP1351 for the treatment of chronic myeloid leukemia.

The FDA granted priority review to a new drug application for CC-486 for the maintenance treatment of adult patients with acute myeloid leukemia based on efficacy and safety results from the pivotal phase III QUAZAR AML-001 study.
The ongoing trial is treating patients with relapsed or refractory CLL/SLL or NHL who failed or were intolerant to 2 or more lines of established therapy, or for whom no other treatment options are available.

The FDA granted regenerative medicine advanced therapy designation to tisagenlecleucel for an investigational new indication to treat patients with relapsed or refractory follicular lymphoma.

The FDA approved ibrutinib in combination with rituximab for the initial treatment of adult patients with chronic lymphocytic leukemia/small lymphocytic lymphoma.
The International Lymphoma Radiation Oncology Group laid out a set of emergency recommendations for alternative radiation treatment schemes for treating patients with hematologic malignancies during the COVID-19 pandemic.
Researchers found that the potential availability of CAR T-cell therapies for large B-cell lymphomas with lower adverse event rates that are suitable for outpatient administration may reduce the total costs of care.
AstraZeneca announced it will be conducting a global clinical trial, CALAVI, to examine the impact of adding acalabrutinib to best supportive care for patients who are severely ill with the COVID-19 infection.
Michael L. Grossbard, MD, suggested that chemo-free regimens, including PI3K inhibitors and a more widespread use of allogeneic stem cell transplant, are being explored as treatment options in this space.
Researchers found that in patients with chronic lymphocytic leukemia receiving commercial ibrutinib, initial dose and dose modification during therapy did not appear to impact event-free survival or overall survival.
A 1-year follow-up of the phase II ZUMA-2 study found that KTE-X19 induced durable remissions in a majority of patients with relapsed or refractory mantle-cell lymphoma.

The FDA granted fast track designation to ME-401, an investigational selective oral inhibitor of PI3K delta, for the treatment of adult patients with relapsed or refractory follicular lymphoma.
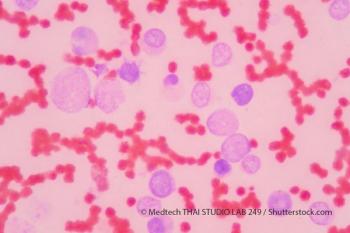
Genentech recently announced their phase III study resulted in improved overall survival and composite complete remission rates for patients with previously untreated acute myeloid leukemia.

Previously unrecognized genetic structural variants in childhood leukemias could be used to evaluate the presence of minimal residual disease during chemotherapy and help to determine response to various therapies.
Hematopoietic stem cell transplantation (HSCT) with prior use of checkpoint inhibitors was found to be feasible in patients with acute myeloid leukemia and/or myelodysplastic syndromes and the use of post-HSCT cyclophosphamide as graft-versus host disease prophylaxis improves outcomes.

A study showed that adolescents and young adults with certain types of cancers saw significant improvements in their 5-year mortality rates, while other cancer types saw little to no significant improvement among the same demographic group.
The associate professor of hematology spoke with CancerNetwork® about frontline treatments available for patients with chronic lymphocytic leukemia and the toxicities present for these treatments.

The FDA granted orphan drug designation to umbralisib based on results from the phase IIb UNITY-NHL trial cohort of patients with follicular lymphoma who have received at least 2 prior lines of therapy, including an anti-CD20 monoclonal antibody and an alkylating agent.
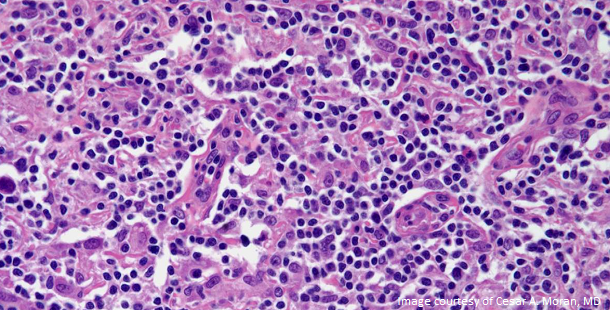
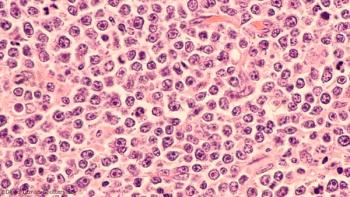
At the 37th Annual Miami Breast Cancer Conference, Valerie Lemaine, MD, MPH, FRCSC, told physicians what they need should know and discuss with their patients about BIA-ALCL.

Kura Oncology’s leading drug candidate, tipifarnib, was granted fast track designation by the FDA to treat adults of T-cell lymphomas.

The new guidelines provide additional guidance for healthcare providers to better recognize and diagnose breast implant-associated anaplastic large cell lymphoma (BIA-ALCL).

The FDA granted priority review to a biologics license application for tafasitamab in combination with lenalidomide for the treatment of patients with relapsed or refractory diffuse large B-cell lymphoma.
This recommendation was based on an analysis of patients with diffuse large B-cell lymphoma undergoing auto-HCT in which the addition of rituximab to the BEAM conditioning regimen had no impact on transplantation outcomes.