Patients with either relapsed or refractory non-Hodgkin lymphoma or chronic lymphocytic leukemia treated with CAR NK cells had a response without the development of cytokine release syndrome, neurotoxicity, or graft-versus-host disease.

Your AI-Trained Oncology Knowledge Connection!


Patients with either relapsed or refractory non-Hodgkin lymphoma or chronic lymphocytic leukemia treated with CAR NK cells had a response without the development of cytokine release syndrome, neurotoxicity, or graft-versus-host disease.

Calibr received approval from the FDA to move forward with an investigational new drug to treat relapsed/refractory B-cell malignancies with a switchable CAR T-cell therapy.
Researchers indicated that a lack of understanding of the mechanism and efficacy of PD-1/PD-L1 inhibitors is the major barrier for prescription of these inhibitors in Chinese tumor treatment-related departments.
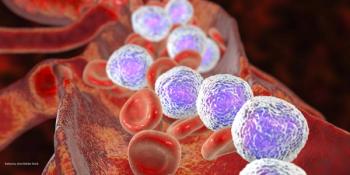
The phase I trial is evaluating cobomarsen in cancers where the disease process appears to be correlated with an increase in miR-155 levels, including adult T-cell leukemia/lymphoma, diffuse large B-cell lymphoma, and chronic lymphocytic leukemia.

Regardless of these improvements though, researchers noted that cancer survivors remain at risk for shorter lifespans, particularly when radiotherapy was utilized as a part of their childhood cancer treatment.
The ALL expert spoke about new research in the field and how it has changed the landscape for this disease.

This is the first cost-effectiveness analysis of the agent compared with the current standard of care using a constructed population-based control arm.

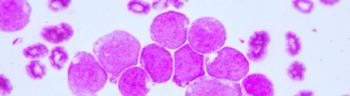
Combined with intensive chemotherapy, the next-generation inhibitor provided excellent results in pediatric patients with Philadelphia chromosome-positive ALL, leading to changes in how this population is treated.
This research has the potential to aid in the development of new strategies for early detection of relapse in pediatric patients with ALL, and the development of treatments to counter clinical occurrence.

Medicare beneficiaries saw unfavorable results when compared to clinical trial participants being treated with idelalisib for their follicular lymphoma or chronic lymphocytic leukemia.

This study indicated that caregivers saw improved quality of life, reduced caregiving burden, lower anxiety and depression symptoms, and improved self-efficacy and coping skills having received psychosocial intervention.

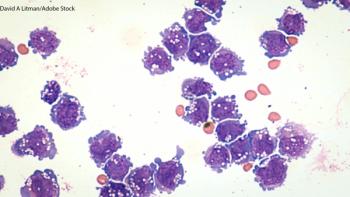
Naval Daver, MD, explains the progress made on 3 abstracts he’s involved with regarding acute myeloid leukemia (AML) at the ASH Annual Meeting and Exposition.
Researchers developed a risk score assessment to measure potential risk for chemotherapy-induced heart failure

Courtney DiNardo, MD, MSCE, elaborated on interim phase II results regarding enasibenib plus azacitidine in patients with newly diagnosed acute myeloid leukemia, and the results from the QUAZAR trial.
The associate professor at The Ohio State University Comprehensive Cancer Center explained the goals for the future of the CAR T-cell therapy data in patients with DLBCL.

The medical oncologist from the John Theurer Cancer Center noted the importance of real-world data in determining potentially different toxicity profiles in these BTK-inhibitors.

Though physical activity guidelines are largely based on chronic diseases like cardiovascular disease and diabetes, these data suggest they are important to cancer prevention as well.

The study evaluating itacitinib in combination with corticosteroids in patients with treatment-naïve acute graft-versus-host disease did not produce statistically significant results.

A phase I study showed brentuximab vedotin combined with a standard chemotherapy regimen of mitoxantrone, etoposide, and cytarabine may be safe and well tolerated in patients with relapsed/refractory acute myeloid leukemia.

Diego Villa, MD, FRCPC, elaborated on the progress made with bendamustine and rituximab as induction therapy for transplant eligible and ineligible patients with mantle cell lymphoma.
The expert hematologist from Plymouth University Medical Center discussed the long-term outcomes of patients receiving ibrutinib for mantle cell lymphoma at the ASH Annual Meeting and Exposition.

The Ohio State University Comprehensive Cancer Center expert discussed the ongoing Alliance A041702 trial at the ASH Annual Meeting and Exposition.
The Willamette Valley Cancer Institute and Research Center expert talks about the results of the ELEVATE TN trial at the ASH Annual Meeting and Exposition.
Bijal D. Shah, MD, discusses the progress made regarding CAR T-cell therapy and mantle cell lymphoma.
