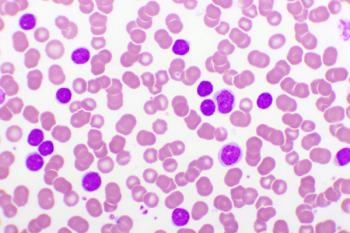
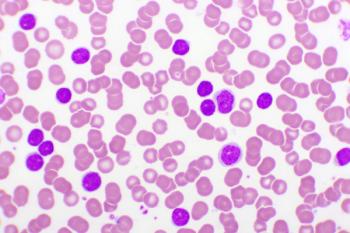
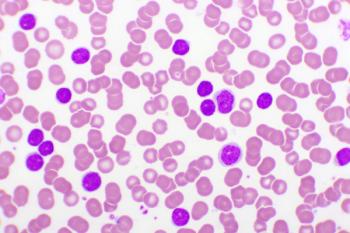
Leukemia
Latest News

Latest Videos

CME Content
More News
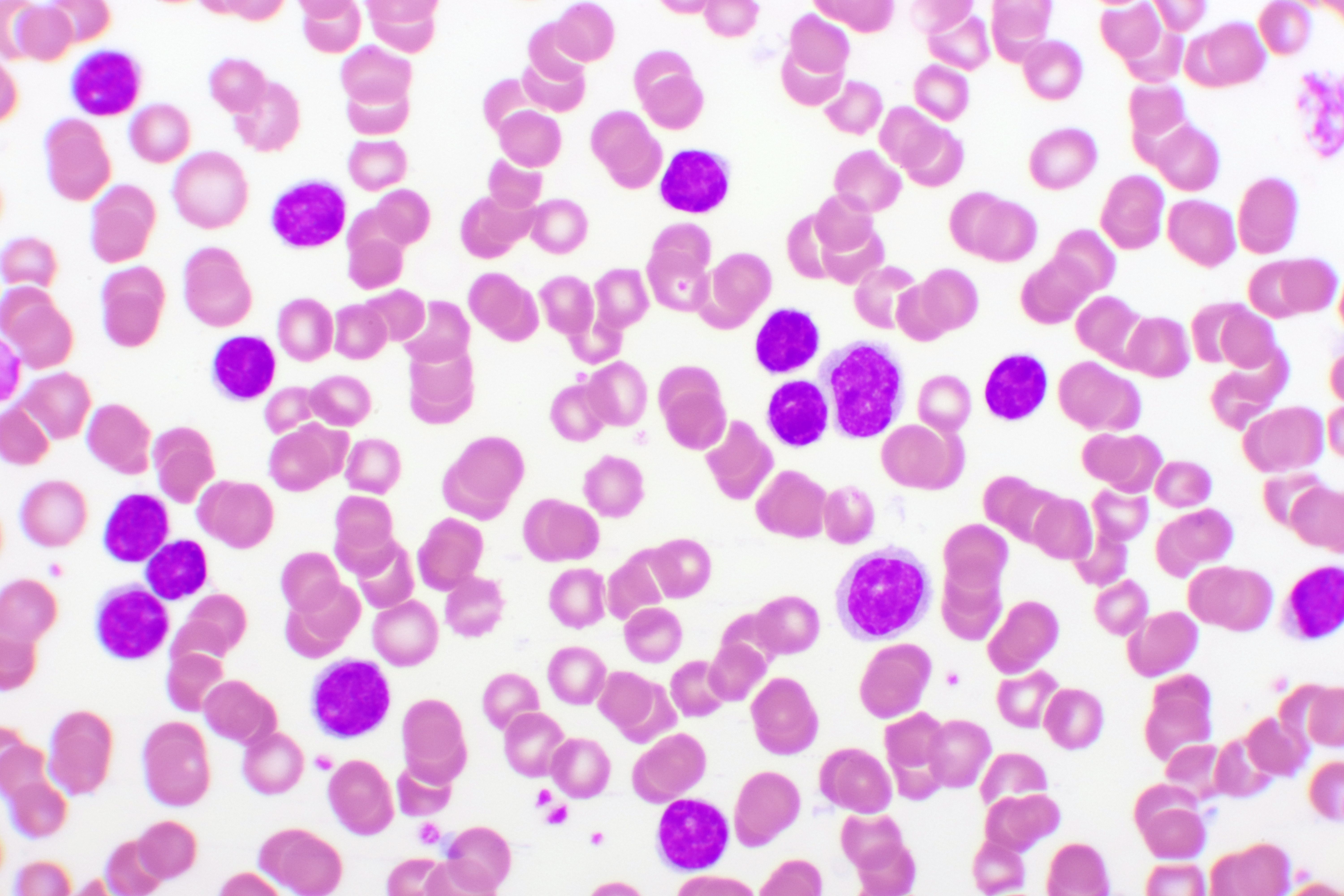
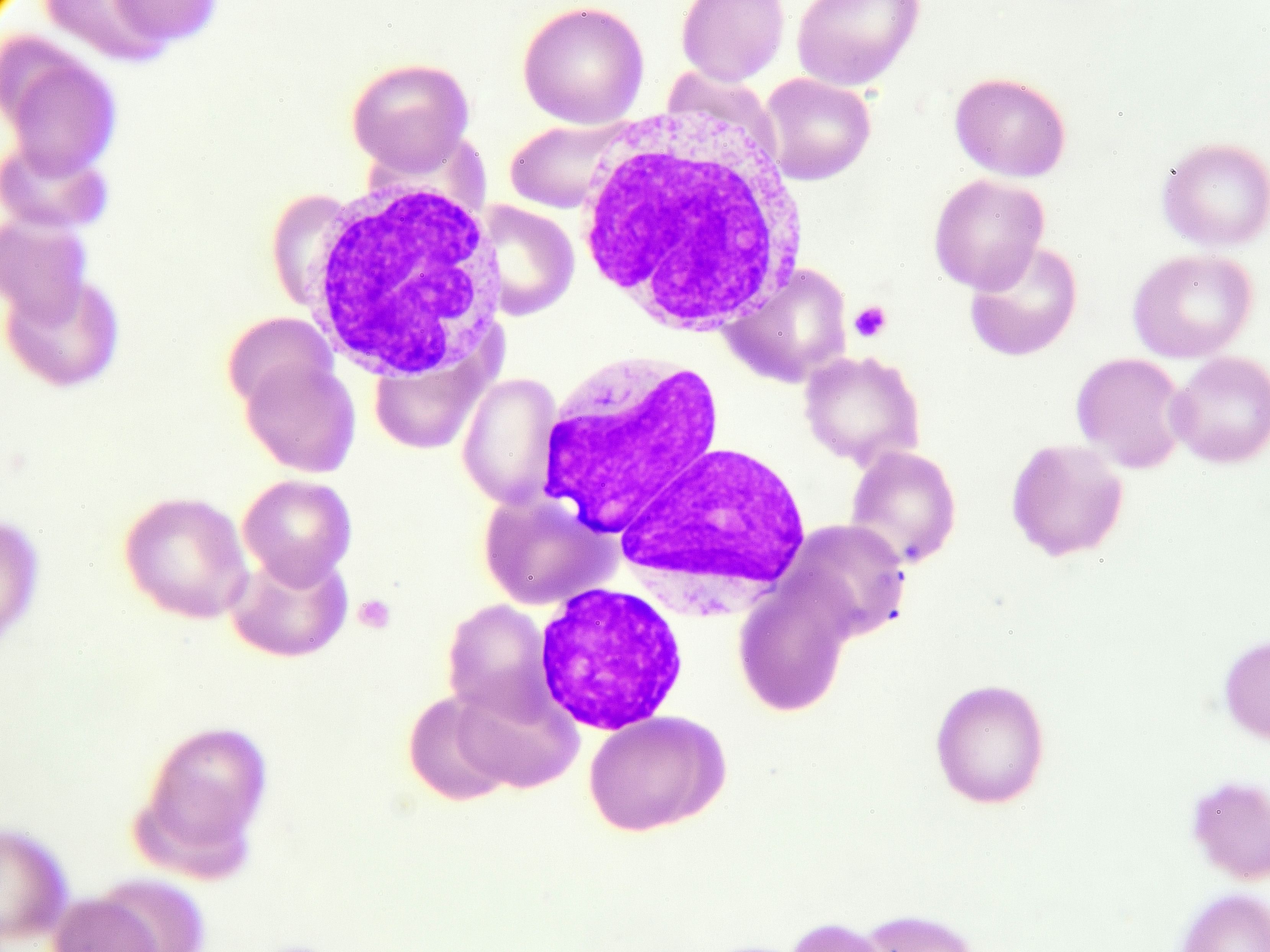
An integrated analysis of 2 phase 3 studies with up to 6.5 years of follow-up reported the outcomes of first-line ibrutinib (Imbruvica) in patients with chronic lymphocytic leukemia and small lymphocytic lymphoma and high-risk genomic features.
This pooled analysis from 4 clinical trials suggested that though patients with TP53 aberrations remain at risk for progression, first-line treatment with ibrutinib has meaningfully improved the poor prognosis in this high-risk population.

Census tract socioeconomic status information demonstrated significant disparities between survival outcomes of non-Hispanic white, non-Hispanic black, and Hispanic patients with acute myeloid leukemia AML in the Chicago metropolitan area.
Azacitidine, was shown to significantly prolong overall survival and relapse-free survival in patients with acute myeloid leukemia in first remission regardless of the number of rounds of prior consolidation therapy.

Treatment with the oral agent showed sustained health-related quality of life compared with placebo in patients with acute myeloid leukemia, according to results of the phase 3 QUAZAR AML-001 trial.
The leukemia expert discussed exciting research being presented at this year’s ASH Annual Meeting.
Following a fixed-treatment duration of ibrutinib combined with venetoclax achieved similar 1-year disease-free survival in patients with previously untreated chronic lymphocytic leukemia/small lymphocytic lymphoma.
Treatment with the combination regimen improved progression-free survival (PFS) and overall survival (OS) over a 5-year period compared with patients treated with bendamustine and rituximab.
The assistant professor of Medicine in the division of Hematology and Medical Oncology at Weill Cornell Medicine spoke about exciting research coming out of ASH for patients with chronic lymphocytic leukemia.
The company expects to complete the rolling submission of its biologics license application for ublituximab in combination with umbralisib in the first half of 2021.
These results suggested that adolescent and young adult patients treated for acute myeloid leukemia have a high risk of developing long-term health complications.
For adult patients with relapsed or refractory T-cell acute lymphoblastic leukemia/T-cell lymphoblastic lymphoma, a phase 1 clinical trial revealed that crenigacestat (LY3039478) demonstrated little clinical activity at the recommended dose.
The study suggested that voriconazole (Vfend) may be the best prophylaxis option for patients undergoing HSCT, and posaconazole (Noxafil) may be the best prophylaxis option for patients with AML or MDS.
The leukemia expert spoke about the importance of genetic testing for patients with acute myeloid leukemia and other important considerations for this patient population throughout the pandemic.

Venetoclax was granted approval in combination with azacitidine, decitabine, or low dose cytarabine earlier this month for adults 75 years or older with newly diagnosed acute myeloid leukemia or those who have comorbidities precluding intensive induction chemotherapy.
Patients who participated in the Beat AML Master clinical trial were found to have superior outcomes with precision medicine, compared to patients with acute myeloid leukemia who opted for standard chemotherapy treatment.

The FDA granted regular approval to venetoclax (Venclexta) in combination with azacitidine, decitabine, or low-dose cytarabine for adults 75 years or older with newly diagnosed acute myeloid leukemia, or who those have comorbidities precluding intensive induction chemotherapy.
The phase 3 ASTRAL-2 and ASTRAL-3 clinical studies evaluated the efficacy and safety of guadecitabine in adults with previously treated acute myeloid leukemia, and with previously treated myelodysplastic syndromes or chronic myelomonocytic leukemia, respectively.
The inherited GATA3 variant rs3824662 was found to strongly influence response to remission induction therapy in childhood acute lymphoblastic leukemia and was also associated with relapse.
Researchers suggested that a scoring system may aid in determining the appropriate use of HSCT in this patient population.
According to researchers, this “group represents more than 20% of children and young adults with ALL, and an increase in attention to adherence, supportive care, and logistics for patients living [more than 50] miles from their treatment center is warranted.”
According to researchers, these “results suggest that both schedules of decitabine are safe and effective in the population assessed.”
Researchers found that long-term treatment-free remission was not impaired by low-dose TKI regimens for patients with chronic myeloid leukemia.

The study was evaluating whether a multicomponent intervention, compared with education alone, would result in a higher proportion of patients with ALL who have mercaptopurine adherence rates of 95% or higher.
The combination was found to be safe and improved overall survival over azacitidine alone in certain patients with acute myeloid leukemia.