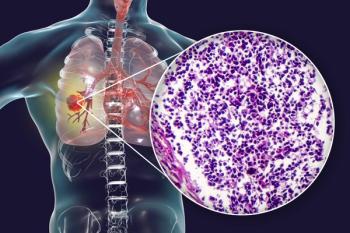
Small Cell Lung Cancer (SCLC)
Latest News
Latest Videos

Podcasts
CME Content
More News

Data from the IDeate-Lung01 trial support the potential role that ifinatamab deruxtecan may play in the management of extensive-stage small cell lung cancer.

Lurbinectedin achieved an ORR of 27% in all patients with extensive-stage small cell lung cancer in the phase 4 Jazz Emerge 402 study.

All efficacy-evaluable patients with ES-SCLC treated with surufatinib, durvalumab, etoposide, and chemotherapy responded to treatment.

After failing to record any objective responses in 9 patients with relapsed/refractory ES-SCLC, the phase 2 trial was terminated early.
Results from the DeLLphi-303 trial showed sustained efficacy and safety with tarlatamab plus anti–PD-1 treatment for patients with extensive-stage SCLC.

Rates of grade 3 or 4 AEs with durvalumab were similar across subgroups, with serious AEs more frequent in patients 70 years or older with ES-SCLC.
The confirmed overall response rate with ABB-706 was 77% in patients with relapsed/refractory small cell lung cancer who received 2 prior lines of therapy.

Leveraging #WCLC25, lung oncologists spoke about the presentations they’re most looking forward to at the upcoming conference.

The median overall survival with atezolizumab plus carboplatin and etoposide was 10.6 months in patients with extensive-stage small cell lung cancer.
The biomarker NLR may not be suitable for prognosis prediction in older patients with small cell lung cancer, according to findings from this real-world study.

No treatment-related deaths were observed with radiotherapy for extensive-stage small cell lung cancer, and most adverse effects were grade 1 or 2.

The median PFS and OS were 5.5 months and 11.2 months, respectively, with nivolumab plus carboplatin/cisplatin and etoposide in patients with small cell lung cancer.
Results from a retrospective study showed that chemoimmunotherapy did not prolong survival vs chemotherapy in a younger ES-SCLC population.

Patients with extensive-stage small cell lung cancer experienced a median PFS and OS of 4.5 months and 7.2 months, respectively, with anlotinib plus irinotecan.
Symptom specificity is now included in updated guidelines for SCLC relating to LEMS, characterized by proximal muscle weakness and autonomic dysfunction.

The field is just beginning to open the door for cellular therapy in lung cancer and other solid tumors, according to Daniel R. Carrizosa, MD, MS, FACP.

Explore innovative strategies and emerging therapies transforming small cell lung cancer treatment, enhancing patient outcomes and survival rates.
The investigational agent showed particularly strong efficacy in an ES-SCLC subgroup, with a chemotherapy-free interval of 90 or more days.

The confirmed objective response rate among 56 patients with extensive-stage small cell lung cancer was 87.5%, all of whom experienced partial responses.

Results from a phase 2 study showed a median OS of 10.2 months in all patients with small cell lung cancer who received stereotactic radiation therapy.
Treatment with tarlatamab demonstrated intracranial responses in a real-world cohort of patients with extensive-stage small cell lung cancer.
HTMC0435 plus temozolomide led to an ORR of 24.5%, with a median OS of 12.0 months, in patients with platinum-sensitive and platinum-resistant small cell lung cancer.

The addition of angiogenesis inhibition to immunochemotherapy for untreated extensive-stage small cell lung cancer did not significantly increase toxicity.
Data from a phase 1 trial showed an ORR of 68% and a DCR of 93% with ZL-1310 in those with extensive-stage small cell lung cancer during dose escalation.
The frequency and severity of adverse effects for the combination were consistent with expected safety findings for each individual agent.