Lymphoma
Latest News
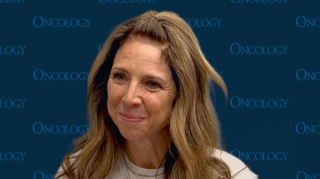
Video Series
Latest Videos
Podcasts
CME Content
More News
Findings from the phase 1/2 BRUIN trial support the Notice of Compliance with conditions for pirtobrutinib in this relapsed/refractory disease population.

Data from a phase 1/2 trial support the FDA’s designation for WU-CART-007 in relapsed/refractory T-cell ALL and T-cell lymphoblastic lymphoma.

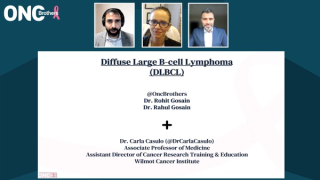
Epcoritamab did not demonstrate a significant improvement in OS, but improvements were observed in PFS, ORR, and DOR in this DLBCL group.

A disease control rate of 100% was attained among 4 patients with Waldenström lymphoma treated with the CAR-NK cell therapy.
The majority of patients with de novo DLBCL who received zanubrutinib plus rituximab and lenalidomide achieved complete responses in a phase 2 trial.
Developers intend to submit a supplemental biologics license application for tafasitamab plus lenalidomide and R-CHOP in this DLBCL population.
Results from arms C and D of the phase 3 SEQUOIA trial demonstrated that zanubrutinib alone or in combination with venetoclax yields positive results in CLL/SLL subpopulations.

Data from the phase 1/2 GO29781 study support the approval of subcutaneous mosunetuzumab in this follicular lymphoma population.

The tafasitamab-based regimen was previously approved by the FDA in June 2025 for patients with relapsed/refractory follicular lymphoma.

The FDA has given a PDUFA date of April 8, 2026, to the nivolumab/AVD regimen for stage III or IV classical Hodgkin lymphoma.
“Compared with pivotal trials, epcoritamab and glofitamab continue to be applied in a broad population of patients with high-risk large B-cell lymphoma,” said Taylor R. Brooks, MD.
Prior bendamustine exposure correlated with worse complete response rates with axi-cel among those with relapsed/refractory follicular lymphoma.
The 3-year event-free survival was 88.9% and 30.0% in patients with high-risk LBCL who did and did not achieve a CR at 6 months, respectively.
Data showed no significant differences in the incidence of CRS and ICANS with the use prophylactic dexamethasone in a retrospective review.
Data from a phase 1/2 trial support sonrotoclax as a promising treatment option in previously treated relapsed/refractory mantle cell lymphoma.

The FDA approved pirtobrutinib as a treatment for patients with CLL/SLL who received prior BTK inhibition based on the phase 3 BRUIN-CLL-321 trial results.
Lenalidomide, tafasitamab, rituximab, and acalabrutinib alone may allow 57% of patients with newly diagnosed LBCL to receive less than the standard number of chemotherapy cycles without compromising curative potential.
The CR/CR with incomplete bone marrow recovery rate was 12.8% in patients with relapsed/refractory CLL/SLL following zanubrutinib treatment.
The phase 3 EPCORE FL-1 trial showed that adding epcoritamab to R2 delivered superior PFS and response rates for patients with relapsed/refractory FL vs R2 alone.
“We can conclude that in combination with dose-attenuated chemotherapy, [epcoritamab] may have a role in the treatment of patients with historically poor outcomes,” said Chan Cheah, MD.

An ORR of 100% was noted in the 160 mg odronextamab/CHOP cohort in untreated DLBCL.
An ORR of 91.4% was observed with zanuburtinib plus R-CHOP in patients with DLBCL.
Over 80% of a small cohort of patients with mantle cell lymphoma achieved a complete response to ibrutinib plus venetoclax.

Treatment with liso-cel led to complete responses in 55.8% of patients with marginal zone lymphoma who received at least 2 prior lines of systemic therapy.

Data from the BRUIN-CLL-321 trial led to the FDA granting traditional approval to pirtobrutinib in CLL/SLL indications.