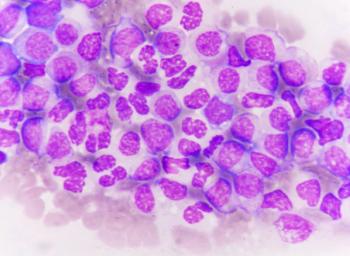
Leukemia
Latest News
Video Series
Latest Videos
Shorts
Podcasts
CME Content
More News
Data from the ENDURE trial may contextualize prior evidence suggesting an interferon-related improvement in treatment-free remission rates in CML.

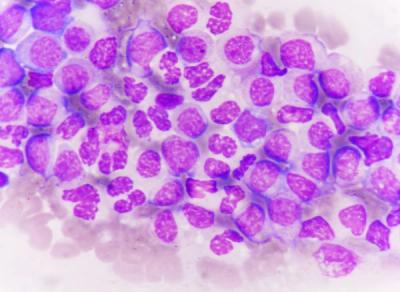
Data from a phase 1/2 trial support the FDA’s designation for WU-CART-007 in relapsed/refractory T-cell ALL and T-cell lymphoblastic lymphoma.
Early safety and immunogenicity data may warrant further evaluation of iTAC-XS15-CLL01 among patients with chronic lymphocytic leukemia.

Data from the phase 1/2 EVICTION study support the breakthrough therapy designation for ICT01 plus venetoclax/azacitidine in acute myeloid leukemia.

Data from the phase 3b ALIDHE study may enrich knowledge on ivosidenib plus azacitidine’s safety and efficacy in IDH1-mutated acute myeloid leukemia.
Results from arms C and D of the phase 3 SEQUOIA trial demonstrated that zanubrutinib alone or in combination with venetoclax yields positive results in CLL/SLL subpopulations.
Data from a phase 1 trial may support additional clinical studies of CT0596 in relapsed/refractory multiple myeloma.

The 1-year EFS with CART19 was 90% among patients with B-ALL who had 1 or more CNS relapses.
Zanubrutinib led to a 72% reduction in the risk of disease progression or death vs bendamustine/rituximab in this CLL/SLL population.

Data from the SEQUOIA trial support the use of zanubrutinib/venetoclax in CLL or SLL regardless of del(17p)/TP53 mutation or IGHV mutational status.
Data from the BRUIN-CLL-313 study may support pirtobrutinib as a new potential standard of care for those with untreated CLL or SLL.

A total of 45% of patients with B-cell acute lymphoblastic leukemia experienced cytokine release syndrome while receiving treatment with MK-1045, of which 3% experienced grade 3 events.

Among patients with NPM1-mutated and KMT2A-rearranged disease, respectively, the ORR was 65% and 41% in the phase 1 KOMET-007 trial.
Ziftomenib given at 600 mg in combination with venetoclax/azacitidine produced high response rates in NPM1-mutated AML.

“Pirtobrutinib continues to show favorable efficacy and promising overall survival [OS],” said William G. Wierda, MD, PhD.

Clinical efficacy and response rates were increased with blinatumomab/ponatinib vs chemotherapy/imatinib for patients with Ph+ ALL.
The CR/CR with incomplete bone marrow recovery rate was 12.8% in patients with relapsed/refractory CLL/SLL following zanubrutinib treatment.

Investigators reported fewer dose reductions due to treatment-emergent adverse effects with pirtobrutinib vs ibrutinib in the phase 3 BRUIN CLL-314 trial.

Azacitidine plus venetoclax reduced the risk of progressive disease, persistent disease prompting therapy change, relapse, hospice, or death by 45%.
Even among Black patients with sufficient social support for clinical trial enrollment, there is inequity related to accessing allogenic transplantation.

Results from a phase 2 trial showed an ORR of 62.5% in patients receiving lisaftoclax monotherapy for CLL/SLL.

A total of 30.0% and 31.5% of families with children undergoing chemotherapy for ALL experienced household material hardship or catastrophic income loss.
Fixed-duration venetoclax regimens with obinutuzumab or ibrutinib showed noninferior PFS vs continuous single-agent ibrutinib in the phase 3 CLL17 trial.

Future work may expand analyses of measurable residual disease as a surrogate end point in AML to the use of modern, non-intensive treatment backbones.

The 2-year EFS end point was met in the cohort of patients given non-TBI conditioning and allogeneic HCT among those with B-ALL who are pre-HCT and NGS MRD-negative.