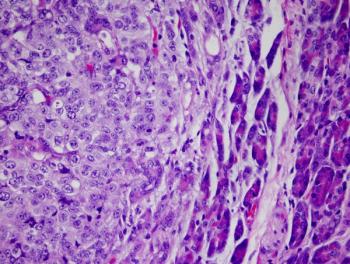
According to findings from the phase 3 PACE-B trial, genitourinary and gastrointestinal toxicities were similar among patients with prostate cancer receiving conventionally fractioned or moderately hypofractionated radiotherapy and stereotactic body radiotherapy.