
All News


Discover key takeaways on tumor markers, the BEP vs. EP debate, and the role of surgery in stage II testicular cancer.

Results from the monarchE study showed a statistically significant OS improvement with abemaciclib plus ET for patients with HR+/HER2– early breast cancer.

Current research initiatives in the kidney cancer field include exploring anti–PD-1, anti–LAG-3, and anti–CTLA-4 combination regimens.

Boris M. Kiselev, MD, provides practical advice for oncology clinicians on how to approach and initiate conversations about a patient’s mental and emotional well-being.

TAS-102 had a significant impact, achieving ctDNA clearance, in patients with colorectal cancer with ctDNA-defined MRD.

Boris M. Kiselev, MD, explores evidence-based interventions for managing cancer-related anxiety and depression.
Data from KEYNOTE-585 showed that adding pembrolizumab to chemotherapy did not negatively impact health-related quality of life vs placebo/chemotherapy.

Results from a pilot phase 2 trial showed that all 5 patients who received treatment achieved a response or had stable disease.

The novel treatment was evaluated in a phase 2 trial and saw a clinical benefit in patients with advanced ovarian cancer.

Declan Walsh, MD, highlighted how the supportive and palliative care space has evolved since he first began working in the field.
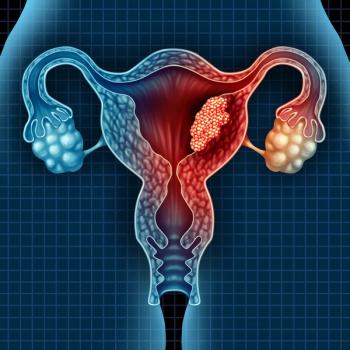
Data from the phase 1/2 RAINFOL-01 trial support the agency’s regulatory decision on rinatabart sesutecan in advanced endometrial cancer.

Boris M. Kiselev, MD, discusses the essential role of psycho-oncology in addressing patient distress, improving treatment adherence, and supporting long-term survivorship.
Two studies were recently published that validated the use of the DecisionDx-SCC test as a tool for the treatment of cutaneous squamous cell carcinoma.

Developers launched a clinical laboratory-developed test version of Haystack MRD in late 2024 and are further expanding access for oncologists.

Both experimental models significantly improved upon historical clinical risk trial groups for patients with acute myeloid leukemia.
Declan Walsh, MD, highlighted the need for nutrition research to enhance oncology care.

Results from the phase 3 VERIFY trial of rusfertide for erythrocytosis in patients with polycythemia vera led to the FDA decision.

Developers will now initiate the phase 3 MarsLight-11 trial of IBI363 among patients with immunotherapy-resistant squamous non–small cell lung cancer.
Being proactive and quickly identifying when a patient may need the supportive care team is the best way to integrate this field into whole-person care.

The median overall survival was 39.3 months with PDS0101 plus pembrolizumab in those with frontline recurrent or metastatic head and neck squamous cell carcinoma.
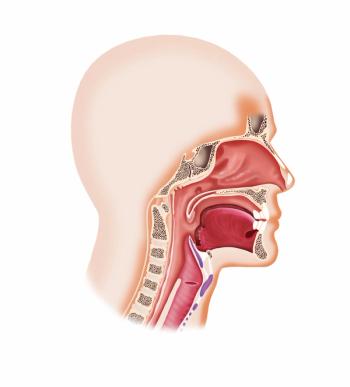
The Chemo Mouthpiece had favorable outcomes when used during and after treatment with chemotherapy among a range of patients with various types of cancer.

Geraldine O’Sullivan Coyne, MD, PhD, MRCPI, discusses how the START center may expand access to novel therapies for patients who reside in a community setting.

The median overall survival with atezolizumab plus carboplatin and etoposide was 10.6 months in patients with extensive-stage small cell lung cancer.

An observational study reported that results with elranatamab for patients with RRMM from the MagnetisMM-3 trial were superior to what was observed across 5 centers in the UK.

Tycel Phillips, MD, highlighted the need for new therapies for patients with MCL who have experienced relapse on previous lines of treatment.
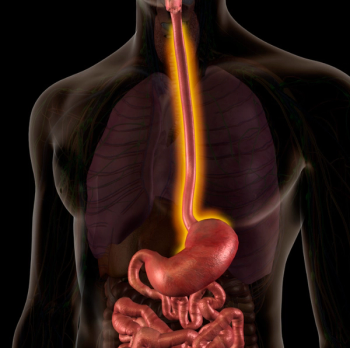
Although radiotherapy was safe and well tolerated in patients with esophageal squamous cell carcinoma, more research is needed to confirm these results.

Tycel Phillips, MD, spoke about the impact the glofitamab CRL had on the landscape of bispecifics in lymphoma.
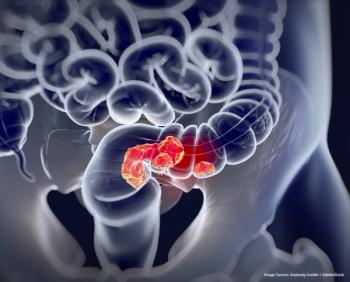
A meta-analysis did not find any correlation between pathologic complete response and overall survival or disease-free survival in patients with rectal cancer.
After the predictive probability of achieving superiority with mFOLFIRINOX or S-IROX was less than 1%, the trial was terminated due to futility.

