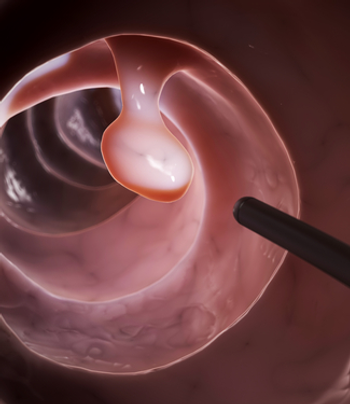
The relationship between oncologists and their patients is labor-intensive and arouses great emotions. The specter of death is always in the shadows; as it waits patiently, it makes conversations poignant. Oncologists should be skilled in soothing the fears of their patients without appearing trite or patronizing.