
Experts cover the regulatory approvals and clinical trial readouts from 2025 that may move the needle for prostate cancer management.

Your AI-Trained Oncology Knowledge Connection!


Experts cover the regulatory approvals and clinical trial readouts from 2025 that may move the needle for prostate cancer management.

The submission of an investigational new drug application for a uPAR-targeted imaging agent, FG001, supports a planned phase 2 trial in glioma.

Data from the phase 2/3 AHEAD-MERIT trial support the FDA decision for this head and neck cancer population.

Treatment with relacorilant plus nab-paclitaxel yielded a 35% reduction in the risk of death compared with nab-paclitaxel alone for patients with platinum-resistant ovarian cancer.
In the ASCENT-04/KEYNOTE-D19 trial, sacituzumab govitecan plus pembrolizumab significantly extended PFS in patients with first-line metastatic TNBC.

Investigators are currently evaluating zavabresib plus ruxolitinib among patients with myelofibrosis in the phase 1 PROMise study.

Neoadjuvant radiation rarely produced RECIST responses, and a significant proportion of tumors increased in size in patients with retroperitoneal sarcoma.

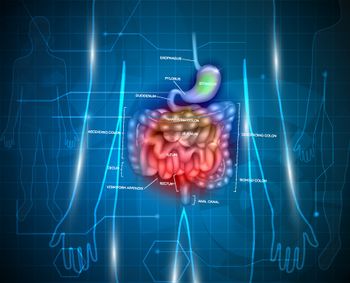
Bezuclastinib plus sunitinib yielded favorable PFS and ORR data vs sunitinib alone in patients with previously treated gastrointestinal stromal tumors.

Throughout 2026, CancerNetwork® and the journal ONCOLOGY® will be dedicated to sharing the most critical developments in the radiation oncology field.

Maveropepimut-S with pembrolizumab and low-dose cyclophosphamide yielded a 40% ORR and 90% DCR in platinum-sensitive high-grade endometrial cancer.

According to the FDA, randomized trials are preferred when assessing MRD to support accelerated approvals in multiple myeloma.

Data from the phase 2 FIRM study support the preliminary potential of firmonertinib as frontline therapy in EGFR L858R-mutated NSCLC.
Caroline Chung, MD, MSc, FRCPC, CIP, explores how AI in diagnostic imaging may help with accelerating scan acquisition and extracting subvisual features.
Caroline Chung, MD, MSc, FRCPC, CIP, discussed how AI is transforming radiotherapy, ranging from uniform dosing to personalized, immune-sparing strategies.

The FDA accepted the NDA for gedatolisib for HR+/HER2–, PIK3CA wild-type advanced breast cancer after it reduced the risk of disease progression or death.
Data from 2 trials at the 2024 and 2025 ASCO Annual Meetings demonstrate the PD-L1/4-1BB bispecific antibody’s efficacy and safety in this population.

The requested information does not pertain to the design or initiation of any new trials, and the developers plan to provide it in the next 30 days.

The folate receptor α ADC yielded responses, with a favorable safety profile, in patients with high-grade serous ovarian cancer in a phase 1 trial.

Updated data from the 5-year analysis of KEYNOTE-942 of mRNA-4157/pembrolizumab in high-risk melanoma showed a maintained benefit.

Toxicities with streptozotocin/5-fluorouracil and everolimus were comparable with other orally available chemotherapeutic schemes in this NET population.

Host Brandon Mancini, MD, MBA, FACRO, introduces a special podcast series focused on delivering key insights and takeaways in the radiation oncology space.

Patients with pancreatic cancer who received up to 6 infusions of the multiantigen-targeted T cell product only experienced 1 treatment-related serious AE.

The marketing authorization was based on results from the DESTINY-Breast09 trial assessing T-DXd/pertuzumab in first-line HER2+ metastatic breast cancer.

Safety data from the phase 1 LUMMICAR study 1 show no high-grade CRS or any-grade ICANS among patients with myeloma who received zevorcabtagene autoleucel.

Investigators used the NCCN Distress Thermometer to identify psychological distress in Nigerian patients with breast cancer in a cross-sectional study.

Epcoritamab did not demonstrate a significant improvement in OS, but improvements were observed in PFS, ORR, and DOR in this DLBCL group.

Pembrolizumab failed to produce clinical responses in patients with recurrent or metastatic medullary thyroid cancer, regardless of prior GI-6207 exposure.

Experts from VCU Massey Cancer Center discuss seamlessly integrating bioimpedance spectroscopy into standard workflows for lymphedema detection.

Data from the phase 2 ALTER-L043 trial may support the viability of perioperative penpulimab-based treatment in resectable non–small cell lung cancer.

Data from CARTITUDE-4 show that cilta-cel can improve outcomes for patients with lenalidomide-refractory multiple myeloma as early as first relapse.