Findings from a health disparities report may support new policies designed to narrow persistent racial and ethnic disparities in health outcomes.

Your AI-Trained Oncology Knowledge Connection!

Findings from a health disparities report may support new policies designed to narrow persistent racial and ethnic disparities in health outcomes.

Collaboration among nurses, social workers, and others may help in safely administering outpatient bispecific T-cell engager therapy to patients.

T-DXd given at 2 dose levels continued to show anti-tumor activity in patients with HER2-overexpressing non–small cell lung cancer.

The primary end point of overall survival was met in the KEYNOTE-811 trial assessing pembrolizumab in HER2-positive gastrointestinal cancer.


Phase 3b data support venetoclax as a treatment option in CLL for patients with or without B-cell receptor–associated kinase inhibitor treatment.

Immunotherapy may be an “elegant” method of managing colorectal cancer, says Gregory Charak, MD.

D. Ross Camidge, MD, PhD, spoke about how the approval of alectinib is the beginning of multiple other approvals for patients with ALK-positive NSCLC.
Biennial screening mammography is recommended for those who are 40 to 74 years old rather than individualizing screening decisions in this age group.

Nurses should be educated on cranial nerve impairment that may affect those with multiple myeloma who receive cilta-cel, says Leslie Bennett, MSN, RN.

Those who have been previously treated for KRAS G12C–mutated advanced NSCLC may benefit from treatment with glecirasib.

Treatment with cilta-cel may give patients with multiple myeloma “more time,” according to Ishmael Applewhite, BSN, RN-BC, OCN.

Safety findings highlight no severe adverse effects or dose-limiting toxicities with the rintatolimod combination in late-stage pancreatic cancer.

Using FOLFIRI as a doublet with durvalumab or a triplet with durvalumab and tremelimumab yielded positive safety in gastric/GEJ cancers.

Nurses may need to help patients with multiple myeloma adjust to walking differently in the event of peripheral neuropathy following cilta-cel.

Amivantamab/chemotherapy has been recommended for approval by the CHMP in advanced non–small cell lung cancer with EGFR exon 20 insertion mutations.

Tisotumab vedotin-tftv may now be given to patients with recurrent or metastatic cervical cancer, according to the FDA.

Patients with overexpressing breast and gastric cancers may now receive trastuzumab-strf, which has been approved by the FDA.
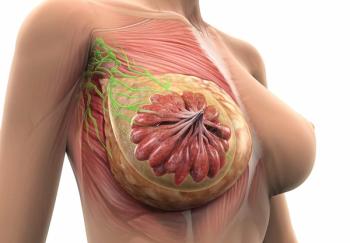
Findings from the phase 3 DESTINY-Breast06 trial will be presented at a future medical meeting and shared with regulatory authorities.

Timothy Chen, MD, highlights how technologies such as ZAP-X and proton therapy may improve outcomes for patients with cancer.
Findings from the CheckMate-901 trial support the CHMP’s positive opinion of nivolumab plus chemotherapy in metastatic urothelial carcinoma.

Nurses must increase the frequency of their assessments for early intervention of patients who undergo treatment for their head and neck cancer, in an effort to truly individualized care.

A mobile app may help to expedite treatment and identification for patients with GVHD.
Additional research may be necessary to validate the efficacy of telehealth interventions in clinical activities for patients with cancer.

Administering neoadjuvant therapy to patients with colorectal cancer may help surgical oncologists attain a negative-margin resection.

Lack of energy, difficulty with sleeping, and pain were some of the most common symptoms reported in older patients with cancer.

Data from 10 new randomized clinical trials support updated recommendations for various systemic therapy regimens in hepatocellular carcinoma.

One of the most important roles of a nurse coordinator is transmitting patient and caregiver information during the CAR T-cell treatment process.

Researchers from MSKCC have explored the potential of personalized fludarabine dosing, based on population pharmacokinetics, to enhance the outcomes of CD19 CAR T-cell therapy in patients with relapsed/refractory aggressive B-cell non-Hodgkin lymphomas.

Researchers at the University of Birmingham in the UK have explored the dynamics of inflammatory biomarkers following allogeneic hematopoietic stem cell transplantation.