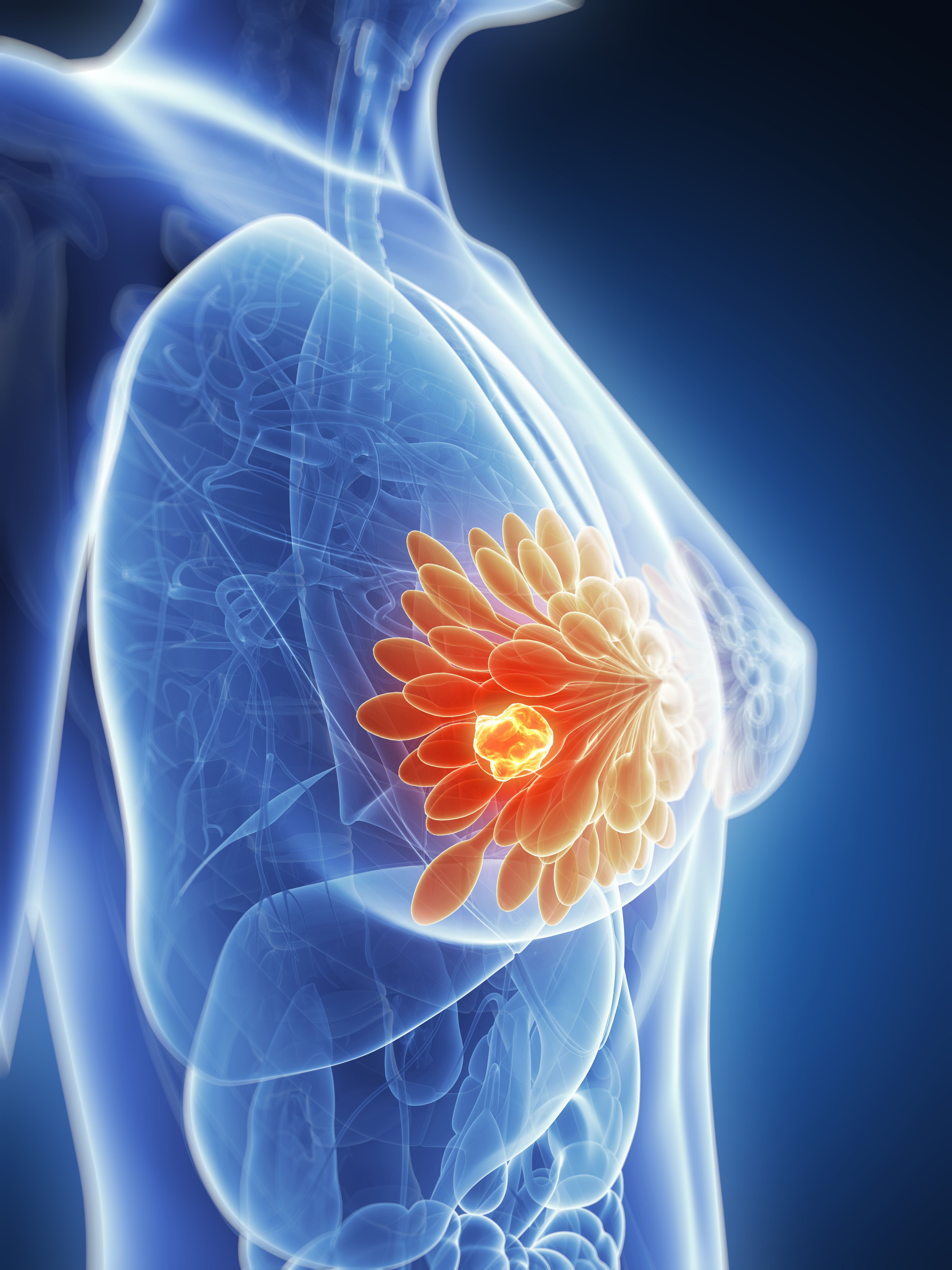
Breast Cancer
Latest News

Resecting MRI-Detected Disease Doesn’t Improve Outcomes in Early-Stage BC

Pembrolizumab/Radiation Improves T Cell Infiltration in Early Breast Cancer
Latest Videos

Podcasts
CME Content
More News
Giredestrant’s safety in the lidERA BC trial was consistent with its known profile, with a lower discontinuation rate vs SOC endocrine therapy.
Axillary dissection was more likely to be omitted among patients in the ALTERNATE trial when there was one positive sentinel node compared with 2 or more.

Across different studies, the highest incidence of left ventricular ejection fraction decrease was seen with trastuzumab/pertuzumab plus chemotherapy.

Explore the latest advancements in antibody-drug conjugates for treating metastatic triple-negative breast cancer and their unique safety profiles.

The safety profile of nadunolimab in patients with triple-negative breast cancer was consistent with its known profile, and no significant signals emerged.

Breast cancer care providers make it a goal to manage the adverse effects that patients with breast cancer experience to minimize the burden of treatment.

According to Rachel Greenup, MD, MPH, some of the barriers to getting optimal treatment for breast cancer include access, insurance, and baseline understanding or knowledge.

Social workers and case managers may have access to institutional- or hospital-level grants that can reduce financial toxicity for patients undergoing cancer therapy.
Insurance and distance to a tertiary cancer center were 2 barriers to receiving high-quality breast cancer care, according to Rachel Greenup, MD, MPH.
According to the developers, giredestrant is the first oral SERD to display beneficial DFS in early-stage breast cancer in the adjuvant setting.

The FDA has approved pertuzumab-dpzb (Poherdy) as a biosimilar to pertuzumab (Perjeta) in breast cancer, based on a review of various attributes, including safety and efficacy data.

Data from the ASCENT-07 trial show an early trend toward improved overall survival with sacituzumab govitecan vs chemotherapy.

Antibody-drug conjugates are effective, but strategies such as better understanding the mechanisms of action may lead to enhanced care for patients with cancer.

Dato-DXd is being assessed in numerous trials across the breast, lung, and bladder cancer spaces.
ADCs demonstrate superior efficacy vs chemotherapy but maintain a similar safety profile that requires multidisciplinary collaboration to optimally treat.
The safety profile of palazestrant plus ribociclib in a phase 1b trial was comparable to prior reports of each individual agent.

Aditya Bardia, MD, highlights the successes and challenges associated with ADC treatments in breast cancer.

Explore the latest advancements in antibody-drug conjugates for treating metastatic triple-negative breast cancer, enhancing patient outcomes and safety.

Explore the promising role of antibody-drug conjugates targeting TROP2 in treating metastatic triple-negative breast cancer and improving patient outcomes.

Onco-dermatology enhances patient care and quality of life by addressing skin toxicities in breast cancer treatments through expert management and collaboration.

Presenting investigators at ESMO Congress 2025 highlight findings from clinical trials assessing novel therapeutics across different disease types.

Read about recent advancements in breast cancer treatment, including new therapies and survival data, showcased at the upcoming ESMO 2025 Congress.
Sacituzumab govitecan plus pembrolizumab reduced symptom burden and improved functioning across multiple domains in the KEYNOTE-D19 study.

Datopotamab deruxtecan significantly enhanced survival rates in first-line treatment for metastatic triple-negative breast cancer.

Policies aimed at improving health coverage and financial assistance may help improve treatment affordability to ensure more equitable survival.