One of the largest whole-exome sequencing analyses in breast cancer is published this week in Nature, identifying a new gene fusion among a subset of triple-negative breast cancers.

Your AI-Trained Oncology Knowledge Connection!


One of the largest whole-exome sequencing analyses in breast cancer is published this week in Nature, identifying a new gene fusion among a subset of triple-negative breast cancers.

Researchers at the University of British Columbia in Vancouver, Canada have sequenced and analyzed over 100 triple-negative breast tumors at the time of diagnosis, the first in-depth genomic analysis of this heterogeneous breast cancer subtype.

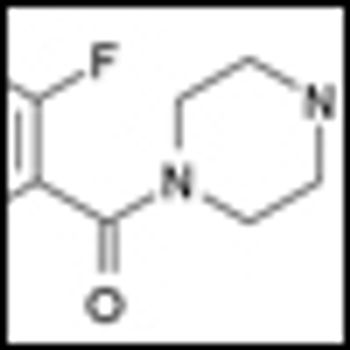
Development of a novel method for drug discovery using active compounds as pharmacodynamic biomarkers in triple-negative breast cancer cell lines.
Researchers have identified a marker of DNA damage that may be able to predict a patient’s response to platinum-based chemotherapy agents such as cisplatin and carboplatin.

Reasons for recurrence after treatment for early breast cancer are still not well understood. Lifestyle and other longer-term factors are likely at play, but the subject is difficult to study. The best advice for cancer patients is exercise and a healthy diet.
What are the latest advances in the treatment of triple-negative breast cancer? Are there new ways to molecularly characterize breast cancer tumors to identify specific mutation targets and increase the chance of response in this disease?

Triple-negative breast cancer is aggressive, has a high rate of metastases, and carries a poor prognosis. Dr. Joyce O’Shaughnessy, who will be presenting at the Miami Breast Cancer Conference, discusses an overview of new therapies for triple-negative breast cancer.

Dr. Gunter von Minckwitz discusses the recent paper he authored that showed that bevacizumab in addition to neoadjuvant chemotherapy significantly increased the rate of pathological complete response in patients with early stage HER2-negative breast cancer.

A study published online in the Journal of Clinical Oncology analyzed triple-negative breast cancer (TNBC) for distinguishing characteristics. The study compared clinical, pathological, and hormone-related lifestyle characteristics of 1469 women aged twenty to forty-nine.

Triple-negative breast cancers represent a challenge for patients and clinicians, with poorer prognosis and fewer treatment options than other breast cancer subtypes. Recently, though, there have been suggestions that targeting pathways that repair DNA within tumor cells could provide benefit beyond the currently available treatments.
Researchers at the BC Cancer Agency in Vancouver and colleagues have just published the results of a phase II study showing that olaparib (AZD2281), an oral PARP inhibitor, may be effective in treating non-BRCA-related ovarian cancer patients.

Researchers at the Vanderbilt-Ingram Cancer Center and the Vanderbilt University School of Medicine have parsed the large and heterogeneous triple-negative breast cancer (TNBC) category of patients into 6 molecularly distinct subgroups. This may be an important step towards delineating these patients as specific genetic subtypes to channel them to appropriate targeted therapy trials.
Triple-negative breast cancer (TNBC) continues to carry a poor prognosis. However, novel prognostic and potentially predictive biomarkers may soon improve that bleak outlook, according to a series of studies presented on Saturday at the American Society of Clinical Oncology (ASCO) Annual Meeting in Chicago.

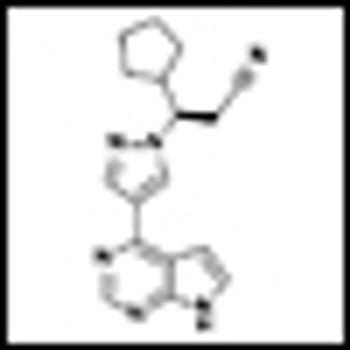
The early promise of treating triple-negative and basal-cell breast cancers with poly (ADP-ribose) polymerase (PARP) inhibitors is yet to be realized, according to Lisa A. Carey, MD, who will be delivering a presentation on treatment options for these patients at the Miami Breast Cancer Conference this week.

The anthracyclines doxorubicin and epirubicin are among the most effective cytotoxic treatments developed for the treatment of breast cancer.

Researchers at Baylor and affiliated institutions reported in the January issue of the New England Journal of Medicine that the addition of iniparib to chemotherapy improves the clinical benefit and survival of patients with metastatic triple-negative breast cancer, without significantly increased toxic effects.

As the FDA considers whether to rescind approval for bevacizumab (Avastin) in the adjuvant setting, “disappointing” results from the GeparQuinto study indicate the agent may be best reserved for patients with triple-negative disease.

For women with triple-negative breast cancer, BRCA mutations can be a boon: These patients have a significantly lower risk of relapse than their counterparts who do not carry BRCA mutations, according to a study out of Houston’s M.D. Anderson Cancer Center. SABCS 2010 will feature an education session on the clinical utility of genetic testing for inherited predisposition to breast cancer.

Although increasing age is the major risk factor for breast cancer incidence and mortality, when adjusted for disease stage, breast cancer mortality is similar among younger vs older patients. Importantly, about 90% of older women with breast cancer present with early-stage disease. The biologic characteristics of breast tumors in older patients suggest they would derive benefit from adjuvant therapy, particularly endocrine therapy, but older women are still frequently undertreated, resulting in poorer survival. Studies suggest that focusing on comorbidity rather than “chronologic age” as a surrogate for life-expectancy is a key aspect of adjuvant decision-making for older patients. Morbidity and mortality from cancer in vulnerable patients with poorer health can be accurately predicted by the Comprehensive Geriatric Assessment (CGA), which evaluates comorbidities, functional status, cognition, social support, psychological state, nutritional status, and polypharmacy. Use of the CGA and newer versions of this tool can lead to interventions that maintain function and improve quality of life in older patients with breast cancer.

None; investigational agents olaparib (AZD2281) and BSI-201 are in phase I and II clinical trials; other PARP inhibitors under investigation include AGO 14699 (Pfizer), ABT-888 (Enzo), and MK4827 (Merck).

As knowledge increases about the processes underlying cancer, it is becoming feasible to design “targeted therapies” directed toward specific pathways that are critical to the genesis or maintenance of the malignant phenotype. Poly(ADP-ribose) polymerase (PARP) inhibitors are an example of this new framework. DNA damage repair is a complex and multifaceted process that is critical to cell survival. Members of the PARP family are central to specific DNA damage repair pathways, particularly the base excision repair (BER) pathway. PARP inhibition, with subsequent impairment of the BER mechanism, may enhance the cytotoxicity of agents that generate single-strand breaks in DNA, such as radiation and certain chemotherapy drugs. In addition, PARP inhibitors may induce death through “synthetic lethality” if the DNA repair mechanisms that rescue BER-deficient cells are themselves impaired. This mechanism is thought to underlie the impressive results of PARP inhibition in BRCA-associated breast and ovarian cancer, and may also account for the reported benefit of this approach in “triple-negative” breast cancer. This review will examine the current understanding of PARP inhibition as a treatment for breast cancer, ongoing clinical trials, and future directions for this new approach.

ORLANDO-Oncologists can expect to hear more about inhibitors of the enzyme poly (ADP-ribose) polymerase-1, or PARP. An experimental agent in this class, BSI-201, prolonged event-free and overall survival in patients with triple-negative breast cancer when used together with gemcitabine (Gemzar) and carboplatin, according to early study results.

Two new studies reported at this year’s ASCO meeting demonstrated the effect of a new class of targeted therapy called poly (ADP-ribose) polymerase (PARP) inhibitors on traditionally difficult-to-treat breast cancers-so-called “triple-negative” breast cancer and BRCA1/2-deficient breast cancers.

Patients with operable triple-negative breast cancer are at increased risk for recurrence if their tumor has higher levels of a protein-encoding gene implicated in migration, proliferation, and other cellular processes, reported Joseph A. Sparano, MD, from the Eastern Cooperative Oncology Group.

In 2008, it is estimated that over 1 million women worldwide will be diagnosed with breast cancer, of which 172,695 will be classified as “triple-negative.”[1] The triple-negative phenotype encompasses a breast tumor subtype that is clinically negative for expression of the estrogen and progesterone receptors (ER and PR) and lacks overexpression of the HER2 protein, with unique prognostic and therapeutic implications.