A study published in JAMA Network Open showed that patient trust in physicians and hospitals dropped from 71.5% in April 2020 to 40.1% in January 2024.

Your AI-Trained Oncology Knowledge Connection!

A study published in JAMA Network Open showed that patient trust in physicians and hospitals dropped from 71.5% in April 2020 to 40.1% in January 2024.

Previously, the phase 2 EVANGELINE trial assessed treatment with (Z)-endoxifen in this patient group.
Developers intend to submit a supplemental biologics license application for tafasitamab plus lenalidomide and R-CHOP in this DLBCL population.

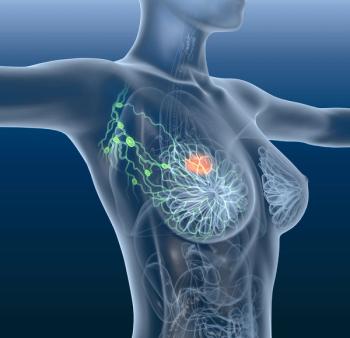
Investigators assessed recurrence rates between axillary lymph node dissection recipients after neoadjuvant chemotherapy vs nonrecipients.

Olvimulogene nanivacirepvec yielded 3 partial responses among 9 evaluable patients with SCLC who had progression or recurrence on prior therapy.

Data from the IZALCO trial support the use of subcutaneous on-body injector administration of an isatuximab-based regimen in relapsed/refractory multiple myeloma.
Emphasizing critical thought over a conformity of thought in oncology may help prioritize and advocate for patients with cancer.

BI-1808 plus pembrolizumab was safe and well-tolerated among patients with recurrent ovarian cancer.
Preclinical data from the phase 2 SUMMIT trial presented at the 2025 ASH meeting support the submission for bezuclastinib in this patient group.

Jose G. Trevino II, MD, FACS, emphasized educating patients and physicians alike to help recognize early signs of pancreatic ductal adenocarcinoma.
Patients with low-risk prostate cancer who have a BMI of 30 or greater experienced a potentially harmful effect after receiving metformin.

Overall survival significantly improved with radiation plus cisplatin/paclitaxel in the phase 2 RTOG 9911 trial over a historical control cohort.

Stereotactic body radiotherapy alone may be feasible instead of immediate systemic therapy in select patients with oligometastatic cancer.

An investigational new drug application for ALA-101 has been submitted to the FDA for the treatment of CD19-positive non-Hodgkin lymphoma and leukemia.
Sorafenib improved the median progression-free survival compared with placebo among patients with metastatic uveal melanoma in the STREAM study.

In patients with cancer, there was an increased risk of cardiovascular death vs those who did not have cancer (HR, 2.46).

Patients currently enrolled on the RAMP 203 trial will have the option of continuing treatment with the avutometinib regimen per investigator discretion.

The approval of narsoplimab by the FDA may now prevent fatal complications from stem cell transplants.
The overall safety profile of melphalan/HDS was comparable among relevant subgroups, with an absence of cumulative toxicity in successive treatment cycles.

Findings suggest a need for interventions to promote equitable use for underrepresented groups and promote PRO use in those with higher symptom burden.
Nurses preferred the FreedomEDGE infusion system compared with the manual push technique in a retrospective survey study.
VCU Massey Cancer Center is utilizing L-Dex bioimpedance spectroscopy to move toward a preventative model for lymphedema.

Frequent follow-up to determine if lymphedema has developed is necessary to catch it early and begin rehabilitation processes.

The use of bioimpedance spectroscopy takes under 2 minutes and can help detect lymphedema before symptoms appear.

Although findings did not show differences in eating restrictions 1 month following gastrectomy, the mobile intervention may help with symptom management.
Data from a phase 2 study may support a novel mTOR inhibitor-based regimen in previously treated, HR-positive, HER2-negative breast cancer.

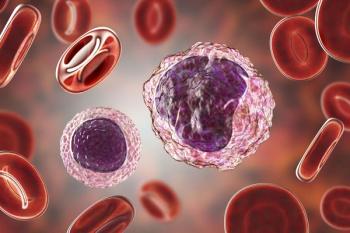
Data from the phase 3b ALIDHE study may enrich knowledge on ivosidenib plus azacitidine’s safety and efficacy in IDH1-mutated acute myeloid leukemia.

The approval of durvalumab plus FLOT for patients with resectable gastric/GEJ cancer cements itself as a new standard of care in the space.
Rahul Banerjee, MD, FACP; and Brooke Adams, PharmD, BCOP, discussed the top hematologic oncology abstracts from the 2025 ASH Annual Meeting and Exposition.
The addition of zovegalisib to fulvestrant led to rapid declines in PIK3CA and ESR1 ctDNA in the HR-positive/HER2-negative advanced breast cancer group.