
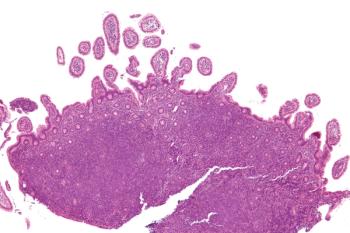
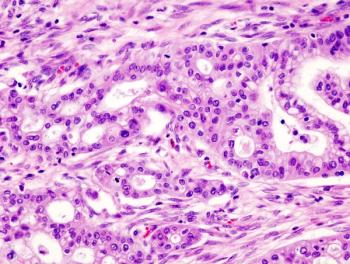
Those immunized between the ages of 12 and 13 in England experienced a significant estimated reduction in cervical cancer and grade 3 cervical intraepithelial neoplasia incidence rates compared with unvaccinated women.

Your AI-Trained Oncology Knowledge Connection!


Those immunized between the ages of 12 and 13 in England experienced a significant estimated reduction in cervical cancer and grade 3 cervical intraepithelial neoplasia incidence rates compared with unvaccinated women.

Patients with invasive HE2-positive breast cancer who were treated with pegylated liposomal doxorubicin plus docetaxel and trastuzumab experienced an increase in a pathological complete response.
CancerNetwork® sat down with Andrew Cook, MD, at the 2021 American Society for Radiation Oncology to discuss outcomes with gabapentin compared with opioids for increasing quality of life and decreasing treatment-related pain in oropharyngeal cancer.
Patients with cholangiocarcinoma may derive benefit from treatment with TT-00420, which was recently given a fast track designation by the FDA.
A phase 1b/2 trial found that the combination of enasidenib plus azacytidine improved overall responses and was well tolerated compared with azacytidine monotherapy for patients with newly diagnosed, mutant-IDH2 acute myeloid leukemia.

UV1 has received fast track designation from the FDA for the use in unresectable or metastatic melanoma.

Research from an observational study suggests it will take time for sexual satisfaction scores to improve among patients with erectile dysfunction due to robot-assisted radical prostatectomy for localized prostate cancer.
CancerNetwork® sat down with Andrew Cook, MD, at the 2021 American Society for Radiation Oncology to talk about using prophylactic gabapentin for those receiving chemoradiotherapy for oropharyngeal cancer.

Patients with hormone receptor–positive, ERBB2-negative advanced breast cancer experienced significant anti-tumor activity when treated with fulvestrant and palbociclib but did not see an improvement in progression-free survival compared with letrozole and palbociclib .

A priority review was granted to toripalimab by the FDA for 2 indications in patients with advanced nasopharyngeal carcinoma.
The FDA granted priority review to a new drug application for parsaclisib in patients with mantle cell lymphoma and other non-Hodgkin lymphomas.
Daniel P. Petrylak, MD, spoke with CancerNetwork® about the results of the TROPHY U-01 study examining sacituzumab govitecan in the treatment of patients with metastatic urothelial carcinoma following failure of platinum-based chemotherapy.

Connie Batlevi, MD, PhD, detailed important updates in therapies for relapsed/refractory follicular lymphoma in this episode of CancerNetwork’s® podcast.

A phase 2 study found that acalabrutinib monotherapy followed by treatment with venetoclax and obinutuzumab in the frontline setting was highly active and tolerable for patients with previously untreated chronic lymphocytic leukemia despite not meeting the primary end point.
In the first episode of a 4-part series, CancerNetwork® spoke with Wade Iams, MD, about the various first-line treat options that are available for patients with small cell lung cancer.

For Pancreatic Cancer Awareness Month, CancerNetwork® spoke with Allyson Ocean, MD, about how family members of patients with pancreatic cancer should seek genetic testing to determine if they are predisposed to pancreatic cancer.

On or after week 5 of treatment with chemotherapy, trilaciclib reduced the need for supportive care therapies in patients with extensive-stage small-cell lung cancer.
Patients with locally advanced or metastatic biliary tract cancer who received either ramucirumab or merestinib in addition to standard first-line cisplatin and gemcitabine did not experience further survival benefit, although safety remained tolerable.

The presence of neuronal autoantibodies in patients with lung cancer, specifically small cell lung cancer and non–small cell lung cancer, appears to be associated with cognitive impairment.

Yazeed Sawalha, MD, discusses how often autologous stem cell transplant is utilized in patients with mantle cell lymphoma.

Treatment with induction UGN-101 produced durable responses in patients with low-grade upper tract urothelial carcinoma.

Brian Rini, MD, discussed abstracts presented during the 2021 ESMO Congress that will have an immediate impact on prostate cancer.

The FDA granted accelerated approval to asciminib for the treatment of patients with Philadelphia chromosome–positive chronic myeloid leukemia for 2 indications.

Patients with BCG-unresponsive non-muscle invasive bladder cancer may benefit from treatment with avelumab and BCG induction therapy
Yazeed Sawalha, MD, discusses how socioeconomic factors may impact the completion of autologous stem cell transplant in patients with mantle cell lymphoma, as well as impacting clinical outcomes.
Older patients undergoing treatment for B-cell malignancies who contracted the COVID-19 virus were at an increased risk of death vs patients with other cancers under the age of 60 years.
Patients treated with eryaspase for second line advanced pancreatic cancer did not meet the primary end point of overall survival in the TRYbeCA-1 trial.
Scott Tagawa, MD, spoke about the implications of the results from his research on treatment patterns of patients with metastatic castration-sensitive prostate cancer, as well as the need for further studies with other data sets.
The AVENIO Tumor Tissue Comprehensive Genomic Profiling Kit could allow for more accessible genetic testing and result in more personalized treatments.

Although canakinumab, an investigational interleukin-1β inhibitor, plus pembrolizumab did not meet the primary end points for locally advanced metastatic non–small cell lung cancer in the CANOPY-1 trial, it could have potential in certain patient subgroups.