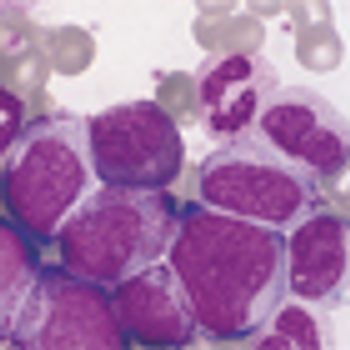
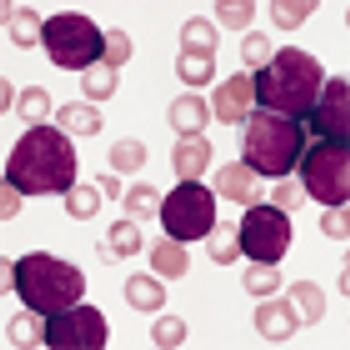
A study from the Mayo Clinic/University of Iowa assessing the use of surveillance CT scans to detect DLBCL relapses found that the majority of relapses occurred outside of regularly scheduled visits and concluded that it is important to educate patients to be more alert to signs and symptoms of relapse.