
An expert from the Mayo Clinic notes that there’s also a great amount of interest in further optimizing the dose of radiation after mastectomy, especially in patients with breast cancer immediately following reconstruction.

Your AI-Trained Oncology Knowledge Connection!


An expert from the Mayo Clinic notes that there’s also a great amount of interest in further optimizing the dose of radiation after mastectomy, especially in patients with breast cancer immediately following reconstruction.

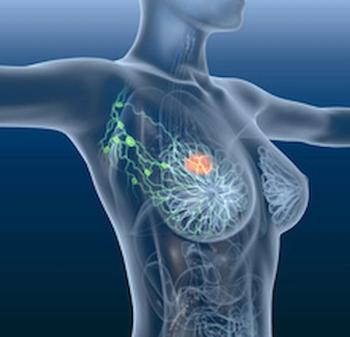
Hypofractionated—large doses of radiation given over a shorter period of time than standard radiation—and conventional proton radiotherapy yielded comparable normal tissue sparing and complication rates postmastectomy in patients with breast cancer, according to findings from a recent study.

Judy C. Boughey, MD, of Mayo Clinic in Rochester, Minnesota indicated that breast conservation therapy, if it can be proven as a reasonable option for patients with multiple ipsilateral breast cancer, could offer patients more choice in treatment.

If feasible, hypofractionated radiation—large doses of radiation given over a shorter period of time than standard radiation—after mastectomy would provide more patients with breast cancer a tissue-sparing option, according to an expert from the Mayo Clinic.

It takes a team of physicians from multidisciplinary backgrounds to best manage patients with contralateral breast cancer, according to a Mayo Clinic Expert.

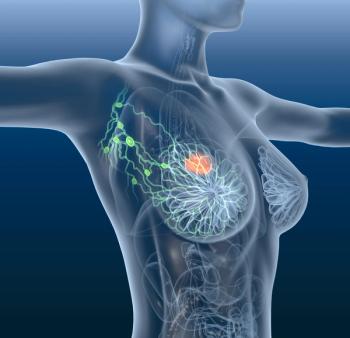
The presence of several risk factors—such as age, race and mutation status—for contralateral breast cancer must be considered when making treatment decisions, according to an expert from the Mayo Clinic.

Recent study findings related to risk factors for developing contralateral breast cancer may better influence treatment decisions between patients and physicians, according to a Mayo Clinic expert.

An expert from the Mayo Clinic discusses findings from a population-based study concerning germline genetic mutations as risk factors of contralateral breast cancer.

An expert from the Mayo Clinic explains why he and his colleagues are researching risk factors for contralateral breast cancer in carriers of moderate-risk genes such as ATM, CHEK2, and PALB2.
Judy C. Boughey, MD; Robert Mutter, MD; and Siddhartha Yadav, MD, MBBS, of Mayo Clinic spoke with CancerNetwork® multidisciplinary findings presented at the 2022 San Antonio Breast Cancer Symposium, ranging from surgery to radiotherapy to biomarker research.

During the 2022 San Antonio Breast Cancer Symposium, Neil M. Iyengar, MD, took over the CancerNetwork® Twitter to review key presentation takeaways.

Patients with HER2-positive metastatic breast cancer experienced promising preliminary safety and efficacy with trastuzumab deruxtecan alone and in combination with pertuzumab.
Improvements in survival were observed in patients with pretreated, endocrine-resistant hormone receptor–positive, HER2-negative metastatic breast cancer who were treated with sacituzumab govitecan vs physician’s choice.
Patients with operable, locally advanced triple-negative breast cancer experienced notable improvements in survival following treatment with neoadjuvant carboplatin plus sequential taxane-anthracycline neoadjuvant chemotherapy.

Long-term findings from the phase 2 GeparOLA trial indicate that olaparib plus paclitaxel and carboplatin did not result in further benefit vs paclitaxel, and carboplatin for patients with HER2-negative, homologous recombination–deficient early breast cancer.

Robert Mutter, MD, of Mayo Clinic says that proton postmastectomy radiation therapy allows for excellent tissue sparing in the management of breast cancer.

Patients with multiple ipsilateral breast cancer might benefit from having a preoperative MRI before proceeding with breast conservation therapy, according to Judy C. Boughey, MD, of Mayo Clinic in Rochester, Minnesota.

Results from the phase 3 STIC CTC trial found an improved overall survival when circulating tumor cells were used as a guide in combination with chemotherapy or endocrine therapy in patients with hormone receptor–positive/HER2-negative breast cancer.

Patients with estrogen receptor–positive, HER2-negative metastatic breast cancer did not derive further benefit when palbociclib was added to fulvestrant.
Patients with ER-positive/HER2-negative metastatic breast cancer had improved progression-free survival when treated with elacestrant compared with standard of endocrine therapy.

Results from the real-world analysis of the phase 2 HER2CLIMB trial showed a good safety profile with the tucatinib triplet regimen in patients with HER2-positive metastatic breast cancer.
ARV-471 monetherapy showed clinical benefit in an expansion cohort of patients with locally advanced or metastatic breast cancer, according to data from the VERITAC trial.

Treatment with a range of camizestrant monotherapy doses resulted in a survival benefit compared with fulvestrant in a post-menopausal patient population diagnosed with estrogen receptor–positive, HER2-negative advanced breast cancer.

Patients with HER2-low or HER2-0 metastatic breast cancer who previously received at least 1 chemotherapy agent garnered similar benefit from eribulin mesylate vs standard physician's choice chemotherapies.

Results from the phase 3 CAPItello-291 trial indicated that the combination of capivasertib plus fulvestrant produced improved progression-free survival in patients who have hormone-receptor–positive/HER2-negative advanced breast cancer.
Trastuzumab deruxtecan improved survival outcomes vs trastuzumab emtasine in patients with HER2-positive breast cancer, according to updated results from the DESTINY-Breast03 trial.
Data from the phase 2 TRIO-US B-12 TALENT trial indicate that fam-trastuzumab deruxtecan-nkxi in the neoadjuvant setting with or without endocrine therapy could be beneficial for patients with hormone receptor–positive, HER2-low breast cancer.

Yoga and conventional exercises also demonstrated long-term improvement in quality of life during treatment for non-metastatic breast cancer, according to results presented at the 2022 San Antonio Breast Cancer Symposium.

Patients with advanced HER2-positive breast cancer had improved progression-free and overall survival when treated with trastuzumab deruxtecan compared with capecitabin-based treatment, according to recent findings.

Experts believe that use of the Breast Cancer Index test in patients with early-stage, hormone receptor–positive breast cancer who are undergoing treatment with endocrine therapy may help to identify those who could be good candidates for the addition of ovarian function suppression.