
San Antonio Breast Cancer Symposium (SABCS)


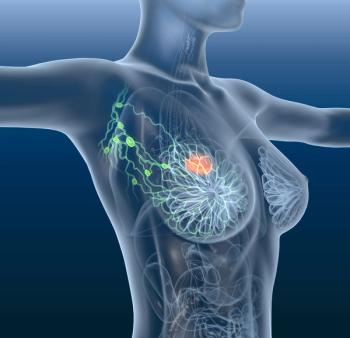
Adding trastuzumab emtansine to tucatinib appears to significantly improve progression-free survival in patients with metastatic HER2-positive breast cancer, says Sara Hurvitz, MD, FACP.

It is important to look at different assays beyond immunohistochemistry to better gather information and potentially predict the activity of trastuzumab deruxtecan in patients with HER2-positive metastatic breast cancer, says Paolo Tarantino, MD.
Combining ribociclib with nonsteroidal aromatase inhibitor treatment also produces relapse-free survival and distant disease-free survival benefits in patients with HR-positive, HER2-negative early-stage breast cancer.

More funding is necessary for additional trials investigating the potential clinical benefit of an alpha-lactalbumin vaccine for patients with high-risk operable triple-negative breast cancer and those at high risk of developing the disease, says G. Thomas Budd, MD.

Treatment with atezolizumab among patients with HER2-positive breast cancer in the phase 3 APTneo Michelangelo trial produces no major tolerability issues, says Luca Gianni, MD.
Findings from a phase 2a study support further development of a regimen including zanidatamab, palbociclib, and fulvestrant in those with HER2-positive, hormone receptor–positive breast cancer.

Latin American patients appear more likely to be diagnosed with aggressive early-stage breast cancer based on factors including metabolics and genetics, according to findings from the FLEX study.

All dose-limiting toxicities with SIM0270 in a phase 1 trial appear to be manageable with dose reductions in those with estrogen receptor–positive, HER2-negative breast cancer.
Investigators observe no new safety signals with trastuzumab emtansine as a treatment for HER2-positive breast cancer after 8 years of follow-up in the phase 3 KATHERINE study.
Administering immunotherapy following surgery in patients with early-stage triple-negative breast cancer does not appear to be as effective as beginning with neoadjuvant treatment, says Peter Schmid, MD, PhD.
Future research may focus on the relationship between neoadjuvant chemotherapy regimens, pathologic complete response, and whole transcriptome changes in patients with hormone receptor–positive, HER2-negative early-stage breast cancer.

Quality of life also appears to be maintained with elacestrant in estrogen receptor–positive or HER2-negative ESR1-mutated breast cancer in the phase 3 EMERALD trial.
Safety findings in the phase 1b DESTINY-Breast08 are comparable with prior reports of trastuzumab deruxtecan and endocrine therapy in HER2-low hormone receptor–positive metastatic breast cancer.
Data from the phase 3 TROPION-Breast01 trial support datopotamab deruxtecan as a potential treatment option for patients with endocrine-resistant, hormone receptor–positive, metastatic breast cancer, says Aditya Bardia, MD, MPH.
Trastuzumab deruxtecan produces the longest time to next treatment in patients with HER2-positive or stable HER2-low advanced breast cancer in the RELIEVE study.

The DEBBRAH trial met its primary endpoint of overall survival in a cohort of patients with HER2-positive or HER2-low advanced breast cancer and leptomeningeal carcinomatosis with positive cerebrospinal fluid cytology.

Heather A. Parsons, MD, MPH, says she is excited about HER2 as a biomarker and investigating the biology of metastatic breast cancer with a minimally invasive liquid biopsy platform.

Data highlight the importance of genomic testing to help optimize treatment and reduce disparities for Black patients with hormone receptor–positive HER2-negative breast cancer, according to Sonya Reid, MD, MPH.
Trastuzumab emtansine plus tucatinib has promising clinical activity and a manageable safety profile in HER2-positive metastatic breast cancer, says Sara A. Hurvitz, MD.

Data from the phase 2 KEYLYNK-009 study indicate a lower rate of treatment-related adverse effects with pembrolizumab plus olaparib compared with pembrolizumab plus chemotherapy in those with triple-negative breast cancer.

The pembrolizumab-based regimen in the phase 3 KEYNOTE-756 trial produces a larger pathologic complete response benefit in patients with node-positive disease and higher PD-L1 expression, according to Joyce O’Shaughnessy, MD.
Preclinical research supports the rationale of combining a BDC-1001 surrogate with pertuzumab to target HER2-expressing tumors.
A future planned analysis of the monarchE trial may further define how circulating tumor DNA dynamics can help identify patients with hormone receptor–positive HER2-negative breast cancer who are at high risk of recurrence.
Combining capivasertib with fulvestrant improves time to deterioration compared with placebo plus fulvestrant among patients with hormone receptor–positive, HER2-negative breast cancer in the CAPItello-291 trial.

Future-looking models see a large decrease in the cost of running sentinel lymph node assessments when artificial intelligence is used.

Combining ribociclib with endocrine therapy appears to be effective and tolerable for those with hormone receptor–positive HER2-negative advanced breast cancer, including elderly patients.

Judy C. Boughey, MD, of Mayo Clinic in Rochester, Minnesota details the efficacy of breast-conserving surgery in patients with multiple ipsilateral breast cancer.

Judy C. Boughey, MD, of Mayo Clinic in Rochester, Minnesota, details the multidisciplinary work that goes into delivering breast-conserving therapy for patients with multiple ipsilateral breast cancer.

Judy C. Boughey, MD, of Mayo Clinic in Rochester, Minnesota discusses the incidence of complications and patient-reported outcomes associated with breast conservation therapy for multiple ipsilateral breast cancer.

