
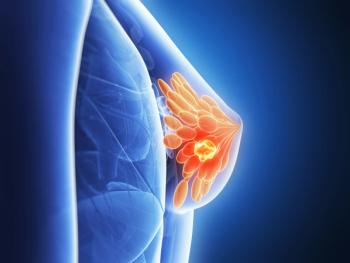
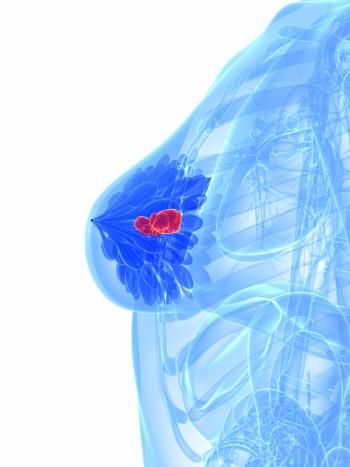
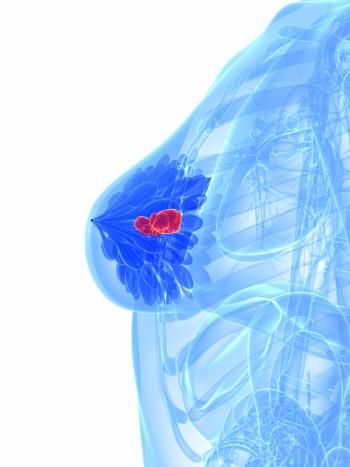
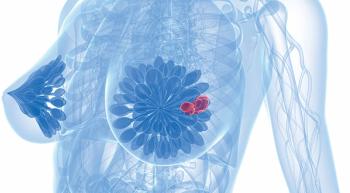
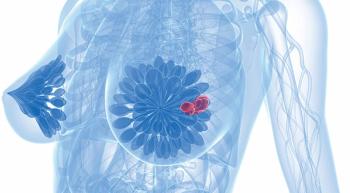
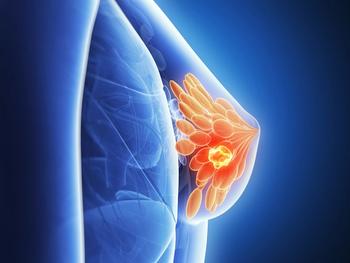
The phase RIGHT Choice trial yield a 46% reduction in disease progression when ribociclib was added to endocrine therapy for patients with pre/perimenopausal hormone-receptor–positive/HER2-negative advanced breast cancer.

Your AI-Trained Oncology Knowledge Connection!


The phase RIGHT Choice trial yield a 46% reduction in disease progression when ribociclib was added to endocrine therapy for patients with pre/perimenopausal hormone-receptor–positive/HER2-negative advanced breast cancer.

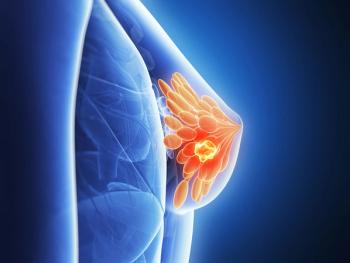
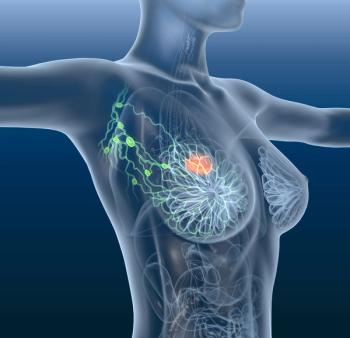
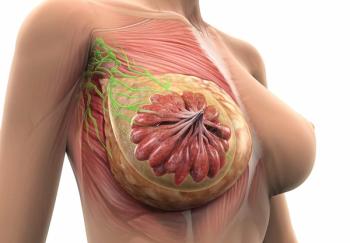
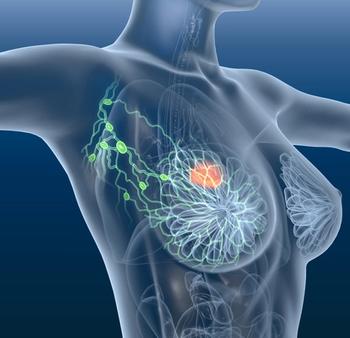
A racial disparity was determined when the tumor microenvironment of metastasis doorway density was found to be higher in Black women vs White women.
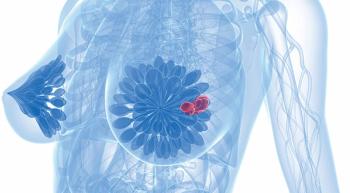
Non-Hispanic Black patients with HR+ breast cancer experienced worse overall outcomes compared with other patient subgroups despite similar recurrence scores, according to a recent analysis of the phase 3 RxPONDER trial.
Everolimus failed to improve survival outcomes when added to adjuvant endocrine therapy in patients with HR+/HER2- breast cancer, according to findings from the phase 3 SWOG S1207 trial.

The prespecified overall survival analysis of the phase 3 monarchE trial when abemaciclib was added to endocrine therapy in patients with hormone receptor–positive, HER2-negative, node-positive early breast cancer.
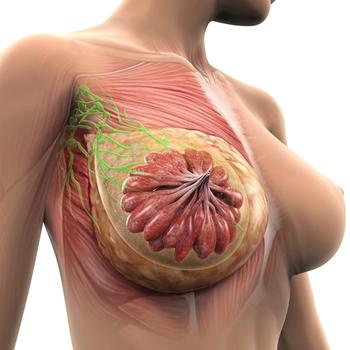
Pre- and postmenopausal women with breast cancer may experience cognitive impairment with chemotherapy and endocrine therapy, which may return to baseline after 36 months.
Patients with HER2-mutant breast cancer given neratinib combinations saw improved efficacy.

Paolo Tarantino, MD, hosted a Twitter Takeover during the San Antonio Breast Cancer Symposium where he discussed abstract presentations and key takeaways in a #CNRealTimeReport.
Research from the 2021 San Antonio Breast Cancer Symposium suggests pathologic complete response and event-free survival were not significantly impacted by race for women with high-risk breast cancer who underwent targeted neoadjuvant chemotherapy.
Patients with gremlin BRCA1/2 mutations and high-risk HER2-negative early breast cancer can have amenable adverse effects after being treated with chemotherapy before utilize olaparib.
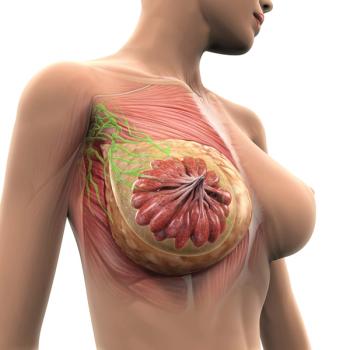
Investigators were able to identify breast cancer immunohistochemistry markers including Ki-67, estrogen receptor, and progesterone receptor status utilizing deep learning–based artificial intelligence algorithms
Patients with hormone receptor-positive breast cancer who were treated with samuraciclib plus fulvestrant saw tumor activity.
Circulating tumor DNA should be utilized early to help detect relapse in patients with triple-negative breast cancer.

Second-line fam-trastuzumab deruxtecan-nxki prolonged survival and led to higher responses over ado-trastuzumab emtansine for patients with HER2-positive metastatic breast cancer.
Patients with HER2-positive breast cancer appeared to derive a higher overall survival benefit after being treated with pyrotinib plus capecitabine vs lapatinib plus capecitabine.
Utilizing neratinib or abo-trastuzumab emtansine for patients with HER2-positive early stage breast cancer reduced the risk of distant recurrence.
The combination of trastuzumab deruxtecan and pertuzumab could improve efficacy over trastuzumab deruxtecan alone for patients with HER2-positive metastatic breast cancer.
Zanidatamab and single agent chemotherapy may hold promise in a population of patients with previously treated HER2-positive breast cancer.
Tucatinib plus palbociclib and letrozole prolonged central nervous system progression-free survival for patients with hormone receptor–positive, HER2-positive breast cancer.
Premenopausal women with hormone receptor-positive, HER2-negative breast cancer saw a survival benefit when treated with adjuvant chemotherapy.
Black patients may have poorer outcomes during breast cancer treatment than White patients.
Data collected from 1400 global laboratories indicate that standard immunohistochemistry testing may not be the most effective method to identify patients with breast cancer with HER2-low disease.

Research presented at the 2021 San Antonio Breast Cancer Symposium highlighted survival improvements for postmenopausal women with hormone receptor–positive HER2-negative advanced breast cancer when treated with ribociclib plus letrozole over placebo.
Those with higher Oncotype DX scores may be more likely to complete the recommended 5 years of endocrine therapy for breast cancer.

Pooled efficacy and safety data confirm that patients who self-identify as Black or Hispanic can be safely treated with palbociclib plus endocrine therapy for hormone receptor–positive, HER2-negative advanced breast cancer.
Patients with early triple-negative breast cancer across prespecified subgroups who were given neoadjuvant pembrolizumab plus chemotherapy followed by adjuvant single-agent pembrolizumab in a phase 3 trial saw an improvement in event-free survival.

Positive response data were seen when patients with advanced or metastatic triple-negative breast cancer were treated with datopotamab deruxtecan.
Results of a phase 3 trial presented at 2021 SABCS indicated that entinostat plus exemestane improved progression-free survival for Chinese patients with advanced hormone receptor–positive breast cancer vs placebo.
Patients with hormone receptor-positive, HER2-negative early breast cancer did not see a benefit when adjuvant palbociclib was added to standard endocrine therapy.

Patients with previously untreated, locally recurrent, inoperable, or metastatic triple-negative breast cancer derived a statistically significant survival benefit following treatment with pembrolizumab and chemotherapy.