
There was no significant difference in the decline in IQ score over time between pediatric brain tumor patients treated with either photon radiation or proton beam radiation therapy, according to a new study.

Your AI-Trained Oncology Knowledge Connection!



There was no significant difference in the decline in IQ score over time between pediatric brain tumor patients treated with either photon radiation or proton beam radiation therapy, according to a new study.

A pooled analysis revealed that the anticonvulsants valproic acid and levetiracetam do not improve progression-free or overall survival in patients with newly diagnosed glioblastoma.

Adult survivors of childhood astroglial tumors with significant vision loss are more likely to suffer various psychological and socioeconomic impacts such as unemployment.

Innovative “adaptive” clinical trial designs are using molecular tools and biomarkers in ways that will streamline research efforts and bring new treatments more quickly to regulatory approval and clinical use.

Expression of programmed death-1 (PD-1) and programmed death ligand-1 (PD-L1) is associated with poor glioblastoma outcomes.

Pregnancy might stimulate tumor growth among women diagnosed with gliomas, according to a single-institution retrospective review of cases.

HLA-A2-positive glioblastoma patients experienced more frequent immune responses to the dendritic-cell immunotherapy IDT-107, responses that may be associated with improved survival.

Adding adjuvant gene-mediated cytotoxic immunotherapy using aglatimagene besadenovec and valacyclovir to standard of care improves survival among patients undergoing surgery for newly diagnosed malignant glioma.

Early results from an ongoing trial suggest that pembrolizumab has promising activity in untreated melanoma patients with brain metastases.

Targeted MAPK-pathway inhibitor therapies appear to have reduced tumor sizes in four children’s inoperable astrocytomas-tumors that had progressed despite chemotherapy.

Adding procarbazine, CCNU, and vincristine to radiotherapy offers pronounced survival benefits for patients with low-grade gliomas harboring IDH1 R132H mutations.

Serum matrix metalloproteinase 9 (MMP-9) and HER2 extra-cellular domain (HER2-ECD) might be predictive biomarkers for the metastasis of breast cancer to the brain, according to a case-control study.

Adding rindopepimut to bevacizumab therapy was associated with improved long-term survival in patients with recurrent EGFRvIII-positive glioblastoma.
Despite promising progression-free survival results, the combination of bevacizumab and lomustine for the treatment of first recurrence in glioblastoma did not improve overall survival, according to findings from the phase III EORTC-26101 trial.

The US Food and Drug Administration announced an expanded indication for the Optune device to treat newly diagnosed patients with glioblastoma multiforme.

A recent study highlights factors that predict worse prognosis for patients with germ cell tumors whose cancer has spread to the brain, including the presence of liver or bone metastases, multiple brain metastases, and others.
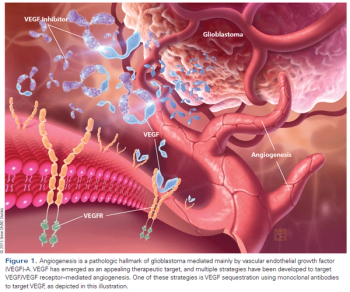
Angiogenesis is a pathologic hallmark of glioblastoma and continues to be an appealing therapeutic target in cancer, including high-grade gliomas.

The absence of any effective combinatorial therapy in patients progressing on bevacizumab and evidence supporting both continuation and discontinuation of bevacizumab in this setting remain important areas for additional clinical trial evaluation in order to better guide our therapeutic decision making in the clinic.

A new genetic analysis found five new genetic variants that raise the risk for gliomas. One of the five was associated with a sharply increased risk for glioblastoma.

A genomic analysis of the primary tumors and brain metastases of patients has revealed potentially targetable mutations only present in the brain metastases.

A new meta-analysis found that adiposity is linked to an increased risk of meningioma, but is unrelated to glioma risk; and physical activity is linked to a lower risk for meningioma.
Gross total resection was associated with significantly lower all-cause mortality in patients with atypical and malignant meningioma, according to a new study.

Often excluded from early trials, adults with high-grade gliomas may be good candidates for solid tumor phase I studies of single agents, according to a new analysis.

Whole brain radiation therapy helps control tumor growth in patients with 1 to 3 small brain metastases, but it does not significantly extend patient survival.

Meningiomas are the most common primary brain tumor and comprise nearly one-third of all newly diagnosed primary brain tumors.