
A phase II trial found that use of a personalized peptide vaccination improved overall survival in patients with chemotherapy-resistant advanced urothelial bladder cancer.

Your AI-Trained Oncology Knowledge Connection!


A phase II trial found that use of a personalized peptide vaccination improved overall survival in patients with chemotherapy-resistant advanced urothelial bladder cancer.

Men diagnosed with prostate cancer who opt for active surveillance/watchful waiting rather than active treatment may not be receiving quality monitoring of their disease.

Following the USPSTF recommendation in 2012 against routine PSA screening, rates of screening and the incidence of early-stage prostate cancer have both declined.

The FDA has approved the anti–PD-1 immunotherapy nivolumab (Opdivo) for the treatment of metastatic renal cell carcinoma.
A 56-year-old man presents with an enlarged prostate. After a biopsy is performed, what is your diagnosis?
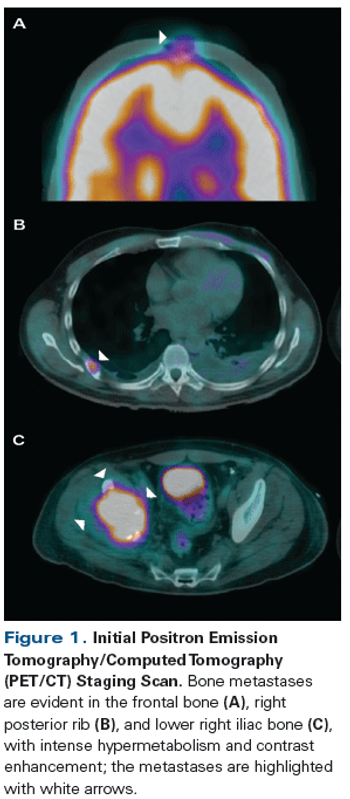
A 42-year-old man presented with increasing right hip pain that limited his ability to walk. Magnetic resonance imaging (MRI) revealed a right lytic acetabular lesion. Further work-up included a computed tomography (CT) scan, which revealed an 8-cm left kidney tumor.
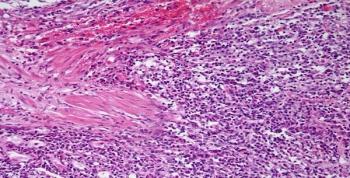
A 63-year-old man complains of blood in his urine. A lesion in the right ureter is identified and a biopsy is performed. What is your diagnosis?

A new study suggests that certain mutagens formed during the cooking of meat are linked to a risk of renal cell carcinoma (RCC).

Researchers have developed a blood test that can identify mutations in the androgen receptor gene that drive resistance to abiraterone. The test could identify prostate cancer patients who will not respond to the treatment.

Patients with renal cell carcinoma whose disease progressed after previous VEGF therapy saw increased delays in disease progression when treated with lenvatinib.

Follow-up of patients with resected non-metastatic RCC should be based on a combination of risk factors for disease recurrence and risk for non-RCC death.

A recent study highlights factors that predict worse prognosis for patients with germ cell tumors whose cancer has spread to the brain, including the presence of liver or bone metastases, multiple brain metastases, and others.

Older patients taking the oral TKIs sorafenib and sunitinib for RCC had a significantly increased risk for cardiovascular events, particularly stroke.

A new meta-analysis suggests that survival outcomes are similar with intermittent and continuous androgen deprivation therapy, and that intermittent therapy may improve some quality-of-life criteria.

Six months of radiation therapy combined with ADT for prostate cancer may not produce a survival benefit in men with moderate to severe comorbidities.

Men with low-risk prostate cancer monitored by active surveillance are not likely to have their disease spread to other organs or die of their prostate cancer.

Despite the clearly established overall health benefits of exercise, its role in reducing prostate cancer risk is unclear. Whereas some studies found often dramatic reductions in prostate cancer risk, others found no effect.
In most cases, localized small-cell bladder cancer requires cystectomy for optimal cure rates.
Radiation therapy with concurrent chemotherapy is an effective treatment strategy for small-cell bladder cancer.

Use of the diabetes drug pioglitazone was not associated with a significantly increased risk of bladder cancer, in a large cohort study.

Patients who have undergone chemotherapy for nonseminoma testicular cancer are at an increased risk for cardiovascular disease, especially in the first year after treatment.

Adding chemotherapy to hormonal therapy in men with metastatic hormone-sensitive prostate cancer increased improved overall survival by 13.6 months.
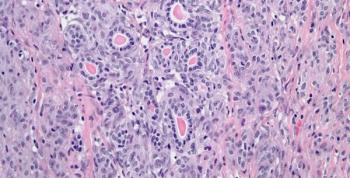
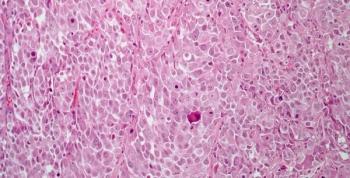
A 20-year-old young man presents with hypertension and a left kidney mass. After further evaluation, a biopsy is performed. What is your diagnosis?

Researchers have identified a subset of six biomarkers that together may predict the risk of more aggressive prostate cancer among African American men.

The 2015 ASCO Annual Meeting delivered new practice-changing results in the area of prostate cancer.